From the very moment the Affordable Care Act’s Medicaid expansion was enacted into law, it faced a wall of opposition – opposition that was strengthened by a Supreme Court decision that allowed states to refuse the expansion.
Despite that opposition, supporters have predicted ever since that states were going to come around eventually – that they would see the positive impact on their residents and that the financial incentives were simply too good to pass up. And the passage of time has certainly proven that true.
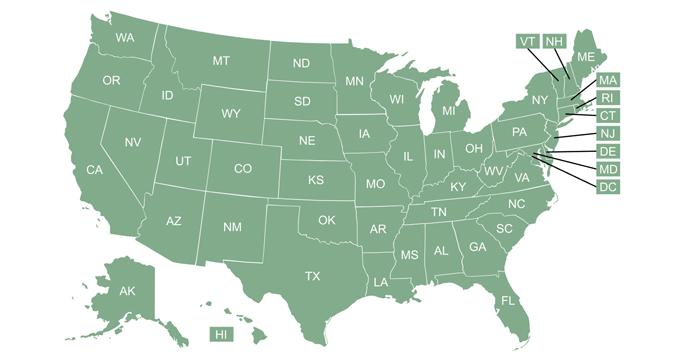
Of the original 26 states that opposed – and initially declined – Medicaid expansion, seven have since changed course. There are now more than 30 states that have made a decision to expand coverage – and several others are discussing plans to expand.
Overcoming opposition arguments
Opponents of the ACA’s Medicaid expansion have often cried foul, claiming that it provides taxpayer-funded health coverage for able-bodied adults who choose not to work, and rely instead on the government for everything from food to shelter – and now health insurance.
It’s true that there’s no work requirement in the ACA’s Medicaid expansion. The idea behind expansion was simply to provide a safety net for people who are struggling financially, including those living in poverty or just above it. (The cap on Medicaid eligibility under the ACA is 138 percent of the poverty level, which is currently less than $28,000/year for a family of three.)
The lack of a work requirement is purportedly one of the reasons some states still haven’t expanded Medicaid coverage. But a new analysis from Families USA highlights the fact that Medicaid expansion has significantly expanded the percentage of working adults who have health insurance.
Rather than looking at the overall uninsured rate, the Families USA study analyzed the change in the uninsured rate for working adults ages 18 to 64. And the results are clearly indicative of the fact that Medicaid expansion increases the percentage of the workforce that has health insurance. These are people who have jobs, and most of us rely on their services (food industry, retail, etc.). But they wouldn’t have health insurance without Medicaid expansion.
In a recent press conference, HHS Secretary Sylvia Burwell noted that “helping people who are working and playing by the rules is something that is an important concept most people agree on” and highlighted the fact that many of the people who are uninsured as a result of states opting out of Medicaid expansion are folks who have jobs.
The Families USA study was based on 2014 data, when 26 states had expanded Medicaid and 24 had not. They found that the national average reduction in the uninsured rate among working adults was 19 percent. 23 states had a higher average reduction, and all but two of them had expanded Medicaid.
Of the 27 states where the average reduction in the uninsured rate among working adults was lower than the national average, 22 were states where Medicaid was not expanded. The visual depiction of the results of the analysis (on page 3 of the report) is striking in terms of how clearly Medicaid expansion is impacting the insurance coverage of the country’s workforce.
Obama’s proposal to entice remaining states
The ACA called for the federal government to fully fund Medicaid expansion from 2014 through 2016, with the states then gradually picking up a small portion of the cost starting in 2017, and paying ten percent of the cost by 2020. (The 90/10 split will remain at that level going forward.)
But that was before states gained the ability to opt out of Medicaid expansion, which didn’t happen until a 2012 Supreme Court ruling. As a result, just 26 states expanded Medicaid as originally scheduled in 2014. To date, 31 states have expanded Medicaid, including Louisiana, where expansion is expected to take effect this year.
So a state that agrees to expand Medicaid starting in 2017 will be on the hook for 5 percent of the cost of expansion from the get-go, because 2017 is the first year that states were to be responsible for a portion of the cost of covering the newly eligible population.
In an effort to entice some of the 19 holdout states to expand Medicaid, President Obama’s budget proposal for the 2017 fiscal year includes a provision – which would have to be approved by Congress – for the federal government to fully fund the first three years of Medicaid expansion in every state, regardless of what years those happen to be. If approved as part of the budget, this would allow a state to expand Medicaid starting in 2017 and not have to begin paying part of the cost of covering the newly eligible population until 2020.
State-by-state details
So what’s going on in the 19 states that haven’t expanded Medicaid? All but two have Republican governors, although nine of the governors (including both Democrats) are at least somewhat supportive of Medicaid expansion in some form.
And several of the states have expansion bills that have been introduced in the current legislative session, although most of the bills face an uphill battle.
If states want ACA funding to expand Medicaid, they must either do so as called for in the ACA, or must obtain approval for modified expansion from CMS under a Section 1115 waiver.
Here’s what’s happening in each state. (Links to legislation include real-time tracking through the legislative process, so you can use this page to see how these bills fare during the legislative session.):
- Alabama – Governor Robert Bentley (R) was previously opposed to Medicaid expansion. But in November he said the state is considering it, although he noted that funding to cover the state’s portion of the cost could be an obstacle. Bentley would prefer that the state obtain a waiver that would allow them to use Medicaid funds to purchase private health insurance for newly eligible Medicaid enrollees. SB182 was introduced on February 9, and calls for a straightforward expansion of Medicaid as laid out in the ACA.
- Florida – Governor Rick Scott (R) has been vocal in his opposition to Medicaid expansion, and Florida lawmakers rejected a Medicaid expansion proposal last June. The 2016 legislative session began January 12, and legal experts don’t expect Medicaid expansion to be a significant issue in this year’s session – although HHS is continuing efforts to get Florida to move forward with expansion. As of early February, no Medicaid expansion bills had been introduced in the Florida legislature.
- Georgia – Governor Nathan Deal (R) is opposed to Medicaid expansion. In mid-January, a legislative panel was split along party lines over Medicaid expansion. Republicans control the state legislature, but in January several Democratic senators introduced SB40 in an effort to repeal language in an existing law that prohibits the state from using any resources to support the expansion of Medicaid. Democratic Senators also introduced SB38, which would provide for state funding for the portion of Medicaid expansion costs the have to be paid by the state. SB368 was introduced in February, and represents the first time a Medicaid expansion bill has gained a hearing by the General Assembly. The legislation doesn’t technically mention Medicaid expansion, but instead calls for a “premium assistance” to help purchase private coverage for people with incomes up to 138 percent of poverty, and would require them to pay up to 5 percent of their income. Obviously, a waiver would be necessary, and the legislation still has a long way to go.
- Idaho – Governor Butch Otter (R) formed a work group in 2014 that has repeatedly supported Medicaid expansion, although Otter himself has stopped short of unequivocal support for expansion. In the 2016 legislative session, two Medicaid expansion bills have been introduced. S1204 would expand Medicaid to everyone with household incomes up to 138 percent of the poverty level, as called for in the ACA. S1205 would implement a modified version of Medicaid expansion (Healthy Idaho), which was recommended by Otter’s work group. S1205 would require a waiver, but the details of the plan have already been pre-approved by HHS. On February 2, the Senate Health and Welfare Committee heard public testimony for the first time regarding Medicaid expansion.
- Kansas – Governor Sam Brownback (R) is opposed to Medicaid expansion, but is willing to consider the possibility of expansion with a waiver, as long as it’s budget-neutral for the state. The House and Senate each have expansion legislation in committee, although lawmakers don’t expect the bills to move to a full vote during this session. The bills (HB2319 and SB371) have been dubbed “The Bridge to a Healthy Kansas.” They are budget neutral, and include a requirement that people with incomes above the poverty level contribute to a health care account each month. But the legislation also has a work requirement (enrollees must be working 20+ hours per week, or else be in school/job training or be a stay-at-home parent), which is not likely to be approved by CMS even if lawmakers pass an expansion bill.
- Maine – Governor Paul LePage (R) is opposed to Medicaid expansion. He has vetoed five expansion bills thus far, and promised in December that he would veto any that are passed going forward. So far, no Medicaid expansion bills have been introduced during the 2016 legislative session.
- Mississippi – Governor Paul Bryant (R) is opposed to Medicaid expansion, and no legislation to expand Medicaid has been introduced in the 2016 session. 79 percent of Mississippi’s 53 rural hospitals are in danger of closing due to financial woes. That’s a far higher percentage than any other state, and the financial difficulties experienced by rural hospitals have been compounded by states’ decisions to opt out of Medicaid expansion.
- Missouri – Governor Jay Nixon (D) supports Medicaid expansion, and has expressed a willingness to go along with Republican proposals that include premiums for enrollees with income above the poverty level, as well as a work requirement. Two identical Medicaid expansion bills (SB961 and SB648) were introduced in the Missouri senate in January, and the same legislation (HB2457) was introduced in the House in February.
- Nebraska – Governor Pete Ricketts (R) is opposed to Medicaid expansion. LB1032, which calls for a privatized version of Medicaid expansion, was introduced in January. LB1032 calls for using federal Medicaid funding to purchase private health insurance for people with incomes up to 138 percent of the poverty level. It also includes optional job training that would be available to enrollees.
- North Carolina – Governor Pat McCrory (R) is somewhat opposed to Medicaid expansion. But he has said he could get behind the idea of expansion if there was a requirement that enrollees be working or actively involved in job training. The 2016 legislative session in North Carolina won’t start until April 25, 2016. But the state is just beginning the process of reforming the existing Medicaid program (as called for in H372, which was signed into law in September 2015). And although public sentiment is starting to lean towards favoring expansion, it’s unlikely that lawmakers will immediately add Medicaid expansion on top of the Medicaid reform that just began.
- Oklahoma – Governor Mary Fallin (R) opposes Medicaid expansion. In February 2016, legislation (SB1372) was introduced to expand Medicaid as called for in the ACA. But the president of the Oklahoma Hospital Association (who supports Medicaid expansion) said in early 2016 that there was “absolutely zero sentiment in the Legislature to even think about expansion of the Medicaid program.” In May 2016, however, another bill – HB3210 – was introduced, calling for an increase of $1.50 per pack in the cigarette tax, with the money to be put into the “Healthcare Revolving Fund.” That would open the door for the money to then be used for a premium assistance program to expand Medicaid using a privatized system like the one used in Arkansas and New Hampshire. However, the legislation doesn’t specifically call for Medicaid expansion, and Oklahoma Democrats refused to pass the measure.
- South Carolina – Governor Nikki Haley (R) is opposed to Medicaid expansion. No legislation has been introduced in the current session to expand Medicaid.
- South Dakota – Governor Dennis Daugaard (R) initially opposed the ACA’s Medicaid expansion, preferring a plan that would only expand coverage to residents with incomes under the poverty level. But by 2015, he was supportive of Medicaid expansion as long as it would be budget-neutral for the state. His proposal includes using federal Medicaid funds to pay for healthcare for Medicaid-eligible Native Americans who receive treatment outside of Indian Health Service facilities. The savings would fund the state’s portion of Medicaid expansion costs. Daugaard’s proposal has received initial approval from HHS, but still has to be approved by tribal leaders and state lawmakers. No legislation on the issue has been introduced thus far in the legislative session.
- Tennessee – Governor Bill Haslam (R) supports Medicaid expansion. But lawmakers have thus far blocked his Insure Tennessee Several measures are under consideration in the 2016 session, including SJR88 (a voluntary “out-out” program that would place Medicaid beneficiaries on private plans, with Medicaid funding to cover premiums and out-of-pocket costs, with beneficiaries eligible to keep any left over funds at the end of the year), SJR103 (a block grant approach to expansion), HB2545 (putting the question of whether to expand Medicaid on the 2016 ballot and letting voters decide), and HJR531/HJR521 (both call for implementation of Insure Tennessee).
- Texas – Governor Greg Abbott (R) opposes Medicaid expansion. Texas has no regular legislative session this year. The coverage gap in Texas is far larger than it is in any of the other states that haven’t expanded Medicaid.
- Utah – Governor Gary Herbert (R) supports Medicaid expansion, but lawmakers have thus far rejected attempts to expand Medicaid, most recently in October 2015. HB275, regarding nonbinding ballot questions, was introduced in February, and paves the way for another bill that would put a nonbinding question regarding Medicaid expansion on the ballot in November. In addition, two Medicaid expansion bills have been introduced: HB18 and SB77. And Republican Rep. Jim Dunnigan is working on legislation that would bypass the ACA’s version of Medicaid expansion, but would extend coverage in the state to some of the “poorest of the poor,” including many homeless people in Utah (edit: this is HB437, which was introduced on February 24 and would extend coverage to about 16,000 residents).
- Virginia – Governor Terry McAuliffe (D) supports Medicaid expansion, but lawmakers have thus far rejected expansion. HB797 was introduced in January, and includes a provision to expand Medicaid. Democrats in the Virginia legislature indicated that Medicaid expansion is still one of their top priorities. The Virginia Hospital and Healthcare Association has also put their support behind expansion, proposing that hospitals pay the state’s portion of the cost of expansion via a provider assessment. But GOP lawmakers in the state continue to resist Medicaid expansion.
- Wisconsin – Governor Scott Walker (R) opposes the ACA’s Medicaid expansion. But Wisconsin is unique among non-expansion states, in that Medicaid coverage there is available to people with incomes up to the poverty level – so there’s no coverage gap. But the state is missing out on federal expansion funding, and will continue to do so until if and when they expand coverage up to 138 percent of the poverty level. AB855 was introduced in February, and calls for – among other things – Wisconsin to obtain the highest available federal matching percentage for Medicaid costs, which would involve expanding coverage. The state would have to submit a financial analysis comparing the cost to the state to cover the population with incomes up to 138 percent of the poverty level versus continuing to fund Medicaid coverage up to only 100 percent of the poverty level.
- Wyoming – Governor Matt Mead (R) supports Medicaid expansion (although that wasn’t always the case), but lawmakers in the state have thus-far rejected expansion proposals, and have acted to ensure that Mead cannot proceed on Medicaid expansion without legislative approval. The 2016 legislative session in Wyoming began on February 8.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.