In this article
Q: My health insurance company is leaving my market. What can I do?
A: If your health insurance company is exiting the market in your area at the end of the year, rest assured that you’ll continue to have other options, and you’ll be able to seamlessly transition to a new plan as of January 1. If you purchased your coverage through the exchange / marketplace in your state, you’ll be automatically re-enrolled in a new plan if you don’t select your own replacement coverage. But it’s important to check your options to evaluate the costs, provider networks and prescription coverage of the plans available to you, rather than relying on the automatic re-enrollment process.
And it’s important to note that all ACA-compliant individual/family health plans follow the calendar year, which means you’d be starting over with a new deductible and out-of-pocket limit on January 1 anyway, even if your existing plan had been renewed.
How widespread are carrier exits?
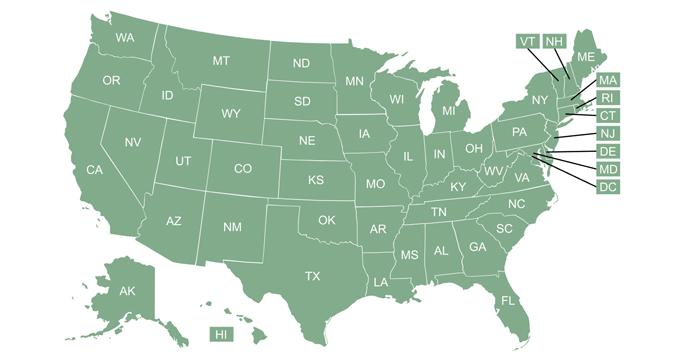
Over the years, carrier exits have been quite common in some years and rare in other years. There were widespread carrier exits in 2017 and 2018, but they were much less common for the next few years (carriers entering the markets became the norm starting in 2019).
There were some significant insurer exits at the end of 2022, including Bright HealthCare, which covers nearly a million people on its individual/family plans across 15 states. And a few other insurers (Friday Health Plans, WPS Health Plan, and Oscar Health) scaled back their participation for 2023 in a handful of states. However, there is also a long list of insurers entering markets in various states for 2023, and the total number of insurers offering plans via HealthCare.gov (the exchange that’s used in 33 states) increased again for 2023.
In most areas of the country, multiple insurers offer individual/family coverage, and you may have dozens or even hundreds of plans from which to choose, depending on where you live.
If your health insurer will no longer offer coverage in your area as of the coming year, it’s important to carefully consider your options and pick a new plan during open enrollment. You have until December 31 to pick a new plan with a January 1 effective date. (This is a special rule for people whose existing plan is no longer available for the coming year. Other enrollees in most states have to finalize their plan selection by December 15 in order to have their coverage take effect January 1).
But it’s in your best interest to get your plan selection finalized by December 15 to ensure that the process goes as smoothly as possible. That will give the insurer time to process your enrollment and get your ID card to you before the start of the new year. It will also ensure that your enrollment goes through the regular channel, instead of having to be processed as a special enrollment period with different effective date rules. In short, enrolling by December 15 will minimize the chances of complications.
Should I let my exchange auto-enroll me in a new health plan?
If you obtained your coverage through your state’s marketplace and your carrier is leaving the market, a type of automatic re-enrollment will be available, but it’s not in your best interest to rely on this process. And automatic re-enrollment is not available if you bought your plan outside of the exchange.
Here’s how this works:
- If you bought your existing coverage through the marketplace in your state, the exchange will select a new plan for you if you don’t take any action. The protocol that’s used in most states essentially moves people to the lowest-cost plan that has the same metal level and product type (HMO, EPO, PPO, or POS) as the plan that’s terminating. (Note that HHS has proposed some changes to this protocol, starting in 2024.)
- If you obtained your existing coverage outside the exchange, there is no entity that can automatically select a new plan for you if your insurer is leaving the market. If you don’t pick your own replacement plan, you’ll be uninsured on January 1.
Even if you have a plan that you obtained through the exchange, you don’t want to rely on the exchange to pick a new plan for you using an automatic algorithm. They won’t be able to prioritize the coverage aspects that are most important for you, which might include considerations like specific medications being covered, specific doctors and hospitals being in-network, having an HSA-qualified plan, or a certain out-of-pocket structure.
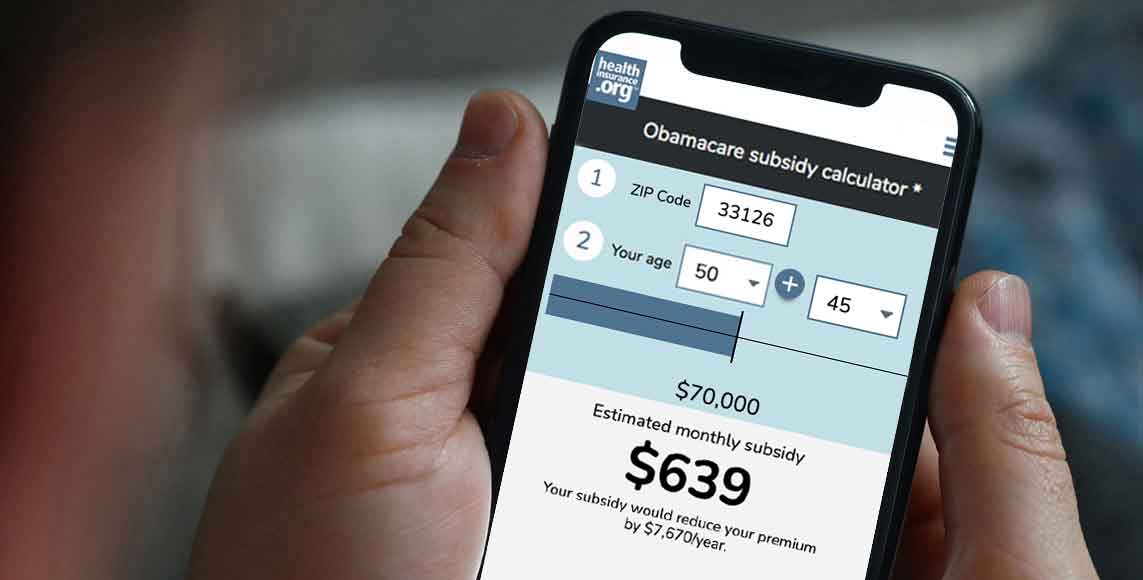
It pays to look at replacement health plan options.
The points discussed above are why it’s so important that you look at all of the replacement plan options that are available for the coming year, and make your own selection. You may find that there are new options that weren’t available this year. And fortunately, the American Rescue Plan’s subsidy enhancements have been extended through 2025, so the larger subsidies that people saw in 2021 and 2022 continue to be available to offset the cost of coverage. The family glitch has also been fixed, making some families newly eligible for subsidies in 2023.
If you don’t get around to choosing a new plan by the end of December, you’ll generally still have a chance to pick a plan in the early part of the new year. (There are some state-run exchanges that may not offer this option if they selected a new plan on your behalf and you didn’t pick a different option by December 31.) The special enrollment period runs for 60 days after the old plan ends.
Although this is better than being stuck with a plan you didn’t choose, enrolling after the first of the year isn’t ideal, as it will mean starting over with a new plan after the year is underway. And if you had off-exchange coverage that terminates at the end of the year, you’ll be uninsured for at least a month if you wait until January to re-enroll, since enrollments after December 31 will generally be effective no earlier than February 1.
Louise Norris is an independent individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org. Her state health exchange updates are regularly cited by media who cover health reform and by other health insurance experts.