In this edition
- COVID-related enrollment window starts Monday in most states
- House committees propose health insurance provisions as part of COVID package
- Virginia House bill would implement reinsurance program in 2023
- Montana House passes bill to prohibit abortion coverage for exchange plans
- South Dakota Senate passes legislation to allow non-insurance Farm Bureau health plans
- State lawmakers introduce Medicaid buy-in legislation
- Biden administration puts Trump-era association health plan rule appeal on hold
COVID-related enrollment window starts Monday in most states
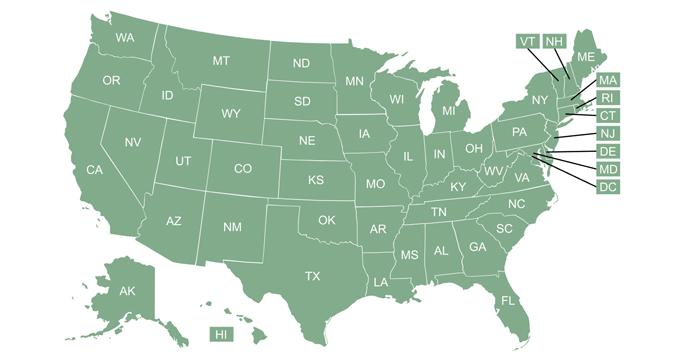
In every state except Idaho, a COVID-related enrollment window will be open by next week — in a few states, they’re already open. (Connecticut announced a COVID-related enrollment window after this week’s Scoop was published, leaving Idaho as the only state without one.) During these enrollment windows, consumers can sign up for ACA-compliant health coverage without a qualifying event.
In most states, the enrollment window applies to anyone eligible to use the marketplace, including people who are already enrolled and want to make a plan change. But some of the state-run exchanges are limiting eligibility to only people who are currently uninsured, or to people who aren’t already enrolled through the exchange. And some states are extending the COVID-related enrollment window to off-exchange plans as well, although financial assistance is never available outside the exchange.
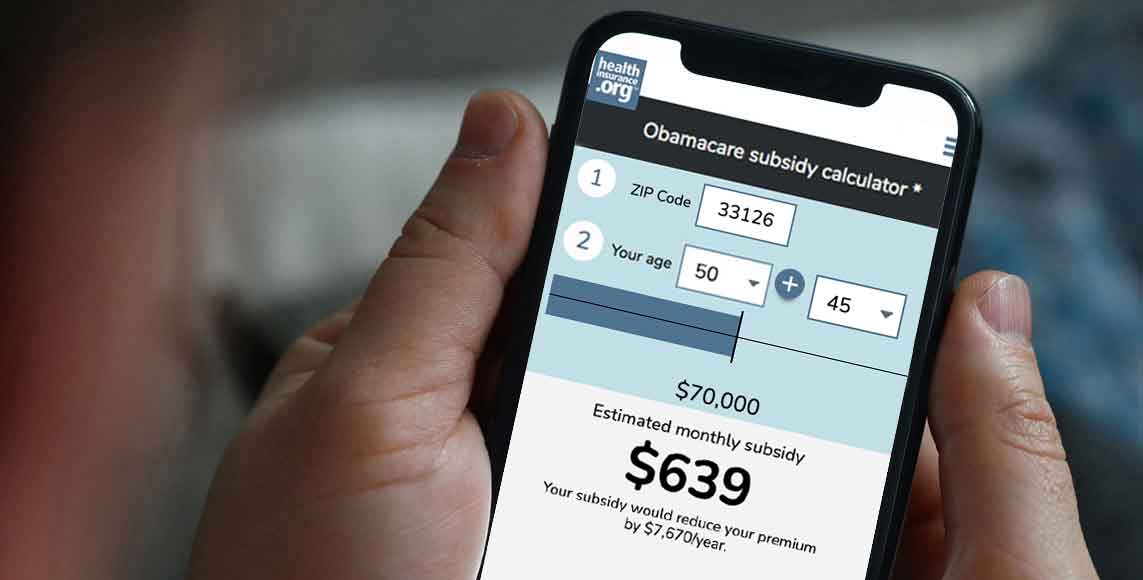
If you’re uninsured or know someone who is, this is an opportunity to have coverage in place for the rest of 2021, with an effective date as early as March 1. Millions of uninsured Americans are eligible for premium subsidies substantial enough to cover the full cost of at least some plans in the marketplace. And Congress is considering COVID relief measures (described below) that would make coverage even more affordable.
House committees propose health insurance provisions as part of COVID package
The House Ways and Means Committee unveiled a set of nine COVID relief proposals this week. Subtitle G, related to “promoting economic security,” includes several important health insurance provisions:
- For 2021 and 2022, the normal rules for the percentage of income a person is expected to pay for on-exchange health insurance would be modified to be much more generous. People with income up to 150 percent of the federal poverty level would pay nothing for the benchmark plan. And nobody would pay more than 8.5 percent of their income, including people who earn over 400 percent of the poverty level (and are currently not eligible for a premium tax credit at all, regardless of how much of their income they have to pay for health coverage).
- For 2020 only, excess premium tax credits would not have to be repaid to the IRS. This is something that several insurance commissioners from around the country suggested to President Biden before he took office. Premium subsidy reconciliation can catch people off guard at the best of times — and 2020 was a particularly complicated year.
- People receiving unemployment benefits in 2021 would receive a premium tax credit that would fully cover the cost of the benchmark plan.
The House Energy and Commerce Committee also published its proposed COVID relief measures this week, including a provision that would provide additional financial incentives for the states to expand Medicaid eligibility if they haven’t already. There are still a dozen states that haven’t expanded Medicaid.
Under current rules, if and when they expand eligibility, the federal government will cover 90 percent of the cost for the newly eligible population, and will continue to fund the rest of the state’s Medicaid program at the state’s normal matching rate (varies from 50 percent to about 76 percent, depending on the state). But under the committee’s legislative proposal relating to Medicaid, states that newly expand Medicaid would get an additional 5 percent federal funding match for their whole Medicaid program, for the first two years of Medicaid expansion.
The committees will markup these proposals this week, and a floor vote in the House on the final COVID relief legislation is planned for later this month.
Virginia House bill would implement reinsurance program in 2023
Legislation was introduced in Virginia last month to create a reinsurance program in the state. Last week, the Virginia House of Delegates passed the bill by a wide margin, and a Virginia Senate committee unanimously agreed to consider the bill during a special session that starts today.
If it’s passed and signed into law, the legislation calls for the state to submit a 1332 waiver proposal to the federal government by January 2022, and for the reinsurance program to be implemented by January 2023. (This is a fairly long timeline. We’ve seen several states implement reinsurance programs over the last few years, often with the program in place for the plan year immediately following the passage of the legislation that authorized it.)
Montana House passes bill to prohibit abortion coverage for exchange plans
Last week, we told you about a bill in Montana’s House that would prohibit on-exchange health plans in Montana from covering abortion services. On Friday, the bill passed in the House by a wide margin, and mostly along party lines. (Four Democrats voted yes, while one Republican voted no.) It’s now with the Montana Senate’s Judiciary Committee for further review. Montana is currently among the minority of states where abortion coverage can be provided under on-exchange plans and at least some plans do offer this coverage.
South Dakota Senate passes legislation to allow non-insurance Farm Bureau health plans
South Dakota’s Senate passed S.B.87 last week, which would allow a nonprofit agricultural organization, domiciled in the state for at least 25 years, to offer non-insurance health benefits to its members. The legislation, which was proposed by South Dakota Farm Bureau, would specifically exempt such health plans from insurance laws or oversight. Tennessee, Kansas, Iowa, and Indiana already allow Farm Bureau health plans to be sold with similar rules. (The plans are not considered health insurance and are thus not subject to insurance laws or regulations.)
The bill is now with the South Dakota House of Representatives, where the Agriculture and Natural Resources Committee approved it 11-1 this week, sending it to a vote on the House floor. The American Cancer Society has expressed strong opposition to the bill, noting that the proposed non-insurance health plans “have the potential of segmenting the insurance market, driving up premiums and making it harder for South Dakotans who live with serious or chronic disease to find health insurance.”
State lawmakers introduce Medicaid buy-in legislation
The concept of Medicaid buy-in as a way of establishing a public option has been debated for several years. Nevada lawmakers passed a Medicaid buy-in bill in 2017, but it was vetoed by the governor. Similar legislation was considered in New Mexico in 2019, but did not pass. (United States of Care has an extensive list of the actions that various states considered in 2019 related to Medicaid buy-in programs.)
This year, lawmakers in several states have introduced various forms of Medicaid buy-in legislation:
- Georgia: S.B. 83/H.B. 214 would create a Medicaid buy-in program that would be available to anyone not otherwise eligible for Medicaid, Medicare, or PeachCare for Kids (Georgia’s CHIP).
- Iowa: S.F. 220 would create a buy-in program for the Hawk-i program (Iowa’s CHIP). It would allow families to purchase coverage for their kids (and young adults up to age 26) through the program if their household income is too high to meet the normal eligibility guidelines. (Currently, 302 percent of the federal poverty level.) The plan would be available through Iowa’s marketplace and could be used with premium tax credits and cost-sharing reductions for eligible enrollees.
- Oklahoma: H.B. 1808 would create a Medicaid buy-in program in the state. The bill would alter the existing Oklahoma statute that directs the state to create a Medicaid buy-in program for people with disabilities if funds become available. The funding aspect is key; Oklahoma has not yet created a Medicaid buy-in program for people with disabilities. But another bill was introduced in Oklahoma last week, calling for the removal of the “if funds become available” language in the existing statute.
- South Carolina: H. 3573 would create a Medicaid buy-in program that would be available to people who are not eligible for premiums tax credits under the ACA, Medicaid, Medicare, or affordable employer-sponsored coverage.
- Tennessee: S.B. 418/H.B. 602 would create a Medicaid buy-in program that would be available to people who are not eligible for premium tax credits, affordable employer-sponsored coverage, Medicaid, or Medicare. (The wording of the Tennessee legislation is very similar to the South Carolina legislation).
Biden administration puts Trump-era association health plan rule appeal on hold
In 2018, the Trump administration relaxed the rules for association health plans (AHPS), allowing self-insured people to join AHPs, as well as small groups that share only a common geographical location. The rules would also have allowed for the creation of these associations for the sole purpose of offering health insurance, without any other business purpose. These rules were soon challenged in court, and vacated by a judge in 2019. The Trump administration appealed the decision, and oral arguments in the appeal were heard by the D.C. Circuit Court in November 2019.
But a ruling had not yet been handed down by the time the Biden administration took office, and the new administration soon asked the court to stay the appeal. The court granted that request this week, so the appeal is on hold while the new leadership at the Department of Labor reviews the case, with status reports due every two months.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.