Home > Supplemental Insurance > Cancer Insurance
See your cancer insurance coverage options.


Financial help during your journey to recovery
The costs of living with cancer are hard to predict. A cancer insurance policy can go beyond your health insurance to provide funds that help cover a wide range of expenses – both medical and non-medical – when you need support most.
According to the American Cancer Society, about one out of every two men and one out of every three women will develop cancer at some point. The medical expenses associated with cancer treatment will generally mean that cancer patients end up having to meet a comprehensive health plan’s deductible and out-of-pocket cap, which can be as high as $9,100 for a single person’s in-network care in 2023.
If you undergo treatment for cancer, you may find that you need to take extended time away from work, and possibly travel to a different area in order to receive the care you need. That can create a significant financial burden – even if you have robust medical coverage.
The financial impact of cancer adds additional stress to an already stressful situation, and a study by Dr. Veena Shankaran, a University of Washington oncologist, and other researchers found cancer patients are 2.5 times more likely to declare bankruptcy than people who haven’t had cancer.
What is cancer insurance?
Cancer insurance, also known as specified-disease insurance in some states, is a type of supplemental health insurance that pays cash benefits for various cancer diagnoses and treatments. You can use that money to pay out-of-pocket medical costs and other expenses, including travel, lodging and meals during treatment, child care and home health services.
Cancer insurance is intended to supplement a comprehensive major medical health plan, and is not suitable to be a person’s only coverage for healthcare.

Frequently asked questions about cancer insurance
How does cancer insurance work?
Unlike major medical policies, which send payments directly to medical providers, cancer insurance policies send benefits to the policyholder (or policyholder’s assignee) to use as they see fit. Cancer insurance plans can pay benefits as a single lump sum, or as a set amount for various specific treatments under a scheduled benefits policy.
- A lump sum policy pays a predetermined amount of money if you’re diagnosed with cancer, regardless of the subsequent treatments that you may need. This can often be added as a rider to a scheduled benefits policy.
- A scheduled benefits policy (also called an indemnity policy) has separate predetermined benefit amounts that you can receive when you have various specific cancer treatments, such as inpatient care, surgery, anesthesia, bone marrow or stem cell transplants, chemotherapy and radiation. (Some plans pay a percentage of incurred costs for specific treatments up to a specified cap, but these are not as common.)
Insurers can offer different levels of coverage, with more expensive policies paying higher benefit amounts. But all cancer insurance policies pay out specified amounts, regardless of your actual costs. This is is why it’s so important to also maintain comprehensive major medical coverage, which does not have a cap on how much it will pay for medically necessary care.
What does cancer insurance cover?
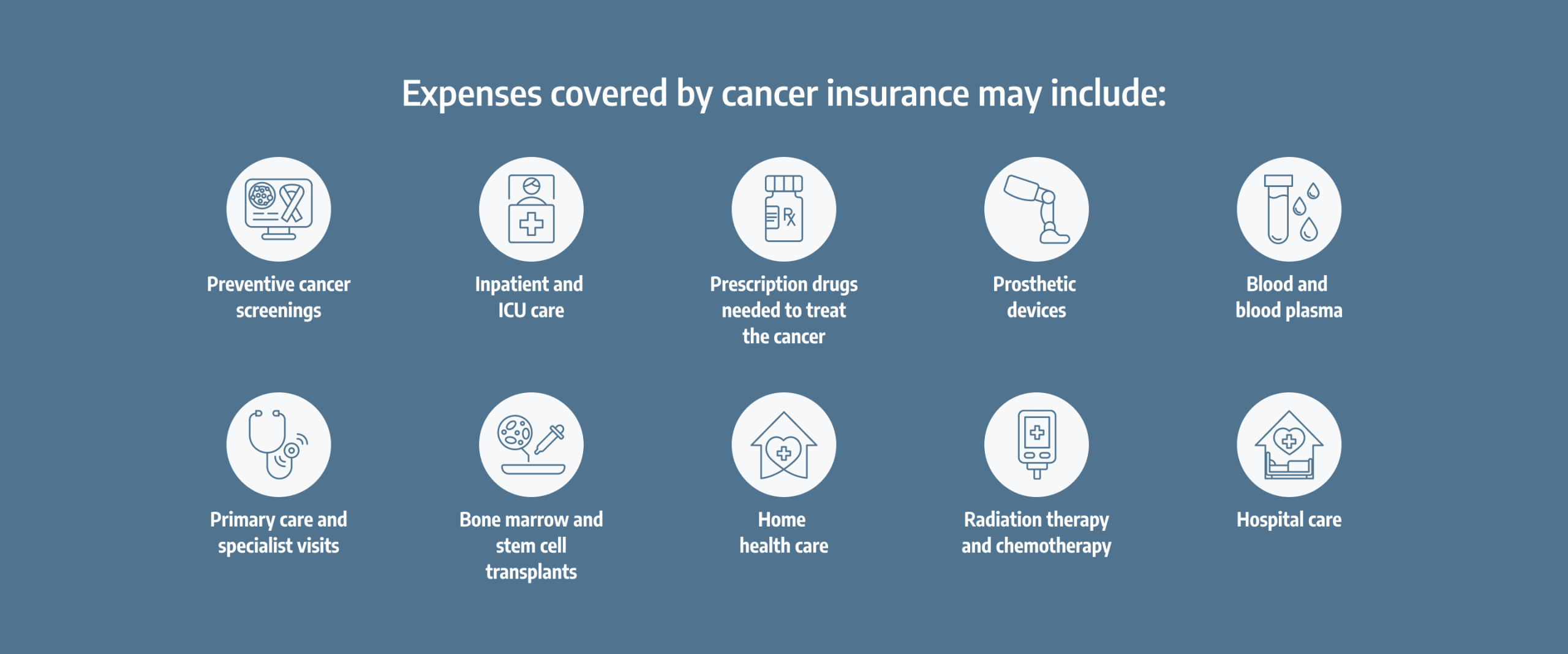
The specifics vary from one plan to another, and each state regulates the benefits allowed by these plans. If a policy pays benefits for specific treatments, it’s common to see payouts for a wide range of medical services, including:
- Preventive cancer screenings
- Inpatient and ICU care
- Surgery, including reconstructive surgery, and any necessary anesthesia
- Prescription drugs needed to treat the cancer or side effects of the treatment
- Radiation therapy, chemotherapy, and immunotherapy
- Bone marrow and stem cell transplants
- Primary care and specialist visits
- Transportation by ambulance
- Blood and blood plasma
- Prosthetic devices
- Skilled nursing and rehabilitation care
- Home health care
- Hospice care
What doesn't cancer insurance cover?
Cancer insurance policies are not designed to cover all of the medical costs a person may incur when they’re being treated for cancer. The average cost of cancer treatment in the first year after diagnosis is $41,800, but total costs can be much higher than that and treatment for some types of cancer can exceed $1 million.
The bulk of the costs for cancer treatment should be covered by a major medical health plan, and no cancer policy can replace the need for major medical coverage.
It’s also important to understand exactly what types of cancer diagnoses or treatments will trigger a payout under your cancer insurance policy. For example, if you find that your cancer coverage only pays benefits for internal cancers, this means it would exclude non-metastasized skin cancer. It’s unlikely that cancer insurance would pay for pre-cancerous conditions. And depending on the policy, benefits for conditions related to the cancer or its treatment may not be part of the coverage.
What factors should I consider when choosing cancer insurance?
Who’s selling the policy?
Make sure the cancer policy insurer (and agent, if you’re using one) is licensed in your state.
Type of payment
Will the policy pay a lump sum if you’re diagnosed with cancer, or smaller amounts for a variety of different treatments?
Conditions covered
Will the plan pay anything if you need treatment for a separate condition that’s related to the cancer or cancer treatment?
Coverage of non-medical expenses
Will it provide a benefit for non-medical expenses, such as child care, pet care/boarding, or travel/lodging?
What companies offer cancer insurance?
There are numerous insurance companies that offer cancer insurance for individuals and families. In some cases, consumers can purchase cancer policies directly from an insurer’s website, while enrollment in other plans – such as employer-sponsored plans – may require the buyer to work with a health insurance agency or brokerage.
Can I get cancer insurance if I already have cancer?
In general, no, unless you’re enrolling in a group cancer/critical illness supplement offered by an employer. (Those plans are generally guaranteed-issue, regardless of medical history.) If you’re buying your own coverage, cancer insurance is something you’d need to purchase before you get cancer.
Thanks to the Affordable Care Act, individual major medical health insurance is guaranteed-issue and covers pre-existing conditions. But supplemental insurance, including cancer policies, is among the excepted benefits excluded by the ACA, and does not have to cover pre-existing conditions. These plans can have waiting periods before benefits can be payable, and they can also deny an application due to medical history.
Depending on the insurer’s underwriting rules, a person who had cancer may have to have been been cancer-free for several years may be able to purchase a cancer insurance policy. It’s important to review the terms of your cancer insurance policy.
Will a cancer insurance policy cover my current doctors?
There are no provider networks for cancer insurance policies, since plans pay benefits directly to the policyholder, who can use the funds for whatever purpose they choose. But to minimize your out-of-pocket costs, it’s in your best interest to use medical providers who are in-network with your major medical health plan.
Is cancer insurance worth it?
This depends on your circumstances. There are several things to consider when you’re deciding whether you should buy a cancer insurance policy:
- How much is your health plan’s out-of-pocket limit, and would having to pay it be a financial hardship?
- Are there more robust health plans available to you, and if so, would it make more sense to spend more on your major medical coverage, instead of supplementing with a cancer insurance policy?
- Do you have a well-funded health savings account (HSA) or emergency fund?
- Do you have a generous paid sick leave policy from your employer, or disability insurance that will cover a portion of your income if you have to take time off work due to cancer treatment?
- If you’re also considering life insurance, do the insurers offer the option to add a cancer rider or critical illness rider to the plan? If so, that can be an economical way to combine life insurance and supplemental health benefits.
- Do you live near good cancer treatment facilities, or is it likely that you might need to travel for treatment?
- Do you have a family history of cancer?
- You know your own circumstances better than anyone. If the financial impact of cancer would likely be stressful, a supplemental cancer insurance policy might add to your peace of mind.
How does cancer insurance differ from critical illness insurance?
Cancer insurance policies will only pay benefits if the policyholder is diagnosed with a covered type of cancer. Critical illness policies (sometimes called “dread disease” policies) are based on a similar concept, but provide benefits for a broader scope of diseases.
Critical illness policies all have specific lists of illnesses that will trigger a payout. Most types of cancer are generally included, along with conditions like heart attack, stroke, or organ failure/transplant.
If the benefit payout amounts are roughly equal, a critical illness policy will generally cost more than a cancer policy, simply because it provides benefits for more medical conditions and thus is more likely to result in a benefit being paid to the policyholder.
If you’re shopping for a cancer insurance policy, you may see the option to add a critical illness rider to the policy. This would increase the premium, but would also expand the scope of medical conditions for which you could receive cash benefits.
Are cancer insurance benefits taxable?
You should contact a financial or accounting professional for guidance about your specific situation. In general, however, the answer depends on whether you got the policy through your employer or purchased it on your own. If you purchase your own cancer insurance policy and pay the premiums with after-tax dollars, benefits you receive under the policy are not taxable. If you’re enrolled in an employer’s group cancer policy and the premiums are paid pre-tax, the benefits can be taxed and you may receive documentation indicating the amount of the taxable benefit that you received.
In 2017, the IRS clarified that if you receive benefits under an employer’s fully insured fixed indemnity benefit plan, you only have to pay taxes on the amount that exceeds your out-of-pocket medical expenses. So, for example, if your health plan has a $25 copay for an office visit and your group cancer policy (paid with pre-tax dollars) pays a $100 benefit for an office visit related to cancer treatment, only $75 of that benefit would be taxable.
But the IRS has proposed new rules in 2023. If finalized, the result would be that benefits received under a fixed indemnity or specified disease policy, without regard for the actual amount of medical expenses incurred, would be taxable if the premiums were paid pre-tax (as is often the case for employer-sponsored supplemental insurance). This would mean the benefits would be subject to FICA, FUTA, and income tax withholding.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.
Footnotes
- Cancer Facts & Figures 2024. American Cancer Society. Accessed February, 2024. ⤶
- A Shopper's Guide to Cancer Insurance. NAIC. Accessed February, 2024. ⤶
- Financial Toxicity (Financial Distress) and Cancer Treatment. National Cancer Institute. Accessed February, 2024. ⤶


