
Medicaid eligibility and enrollment in Iowa
Medicaid enrollment increase of 77% since 2013, but post-COVID disenrollments resume in the spring of 2023

Who is eligible for Medicaid in Iowa
The Medicaid eligibility guidelines in Iowa are as follows (these amounts include a built-in 5% income disregard that’s used for MAGI-based Medicaid eligibility determinations):
- Children up to age 1 in Iowa are eligible for Medicaid in families with income up to 380% of the federal poverty level (FPL)
- Children ages 1 to 18 are covered by Medicaid in Iowa in families with income up to 172% of FPL
- Children in families with income too high to qualify for Medicaid are eligible for the Children’s Health Insurance Program (CHIP); Iowa’s program is named hawk-i, and it’s available to kids with family income up to 307% of FPL
- Pregnant women are covered by Iowa Medicaid if family income is up to 380% of FPL (As of 2023, coverage for the mother only lasts for 60 days after the baby is born. The majority of the states have extended this to 12 months. Although Iowa lawmakers failed to pass legislation in 2022 that would have made that change, similar legislation has again been introduced in 2023. An appropriations bill that Iowa enacted in 2022 called for the state to study the question of expanding postpartum Medicaid coverage to 12 months.)
- Adults under age 65 with incomes up to 138% of FPL are eligible for Iowa Medicaid
Other people, such as low-income elderly, blind or disabled individuals, may qualify for Medicaid in Iowa as well, although there are both income and asset limits for these populations (as opposed to just income requirements for the MAGI-based populations described above). See who qualifies or call 1-800-972-2017 (Relay Iowa TTY: 1-800-735-2942) or email [email protected] for more information.
for 2026 coverage
0.0%
of Federal Poverty Level
Apply for Medicaid in Iowa
Apply online via the Iowa DHS site or HealthCare.gov. Print an application in English or Spanish and mail it to Imaging Center 4; PO Box 2027; Cedar Rapids, Iowa 52406. Call 1-855-889-7985 to get help with your application.
Eligibility: Children up to age 1 with family income up to 375% of FPL. Children ages 1 to 18 with family income up to 167% of FPL; children with family income up to 302% of FPL may qualify for the hawk-i program. Pregnant women with family income up to 375% of FPL. Adults with family income up to 138% of FPL.
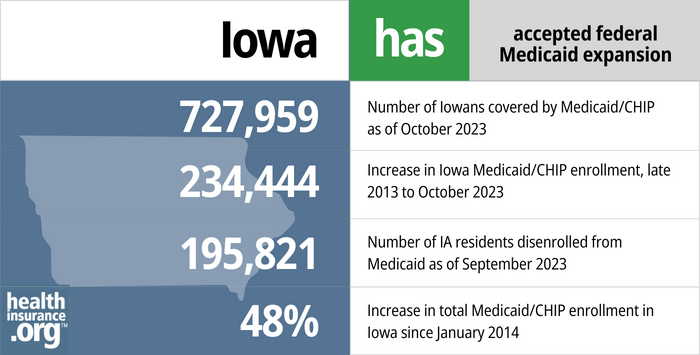
Has Iowa implemented Medicaid expansion?
Iowa’s Medicaid program covers various categories beneficiaries at higher incomes than many other states do, and Iowa expanded Medicaid to low-income adults through the Affordable Care Act (ACA). Initially, the state used a waiver to implement an Iowa-specific version of Medicaid expansion, but that was abandoned in 2015 in favor of straight Medicaid expansion as called for in the ACA, albeit with a managed care approach that utilizes private insurers to provide coverage and care coordination. Medicaid expansion in Iowa is called the Iowa Health and Wellness Program.
- 727,959 – Number of Iowans covered by Medicaid/CHIP as of October 20231
- 234,444 – Increase in Iowa Medicaid/CHIP enrollment, late 2013 to October 20232
- 195,821 – Number of IA residents disenrolled from Medicaid as of September 20233
- 48% – Increase in total Medicaid/CHIP enrollment in Iowa since January 20142
Explore our other comprehensive guides to coverage in Iowa

If you’re looking for an affordable health insurance plan in Iowa, this state guide can help you better understand your coverage options. For many, an Affordable Care Act (ACA) Marketplace plan, also called Obamacare or an exchange plan, is a cost-effective option.


The average family dental premium in Iowa was about $42 per month in 2022.4 Learn about your dental coverage options in the state.


In April 2023, there were 664,712 Medicare beneficiaries in Iowa.5 Use our guide to learn about Medicare, Medicare Advantage, and Medigap plans available in Iowa.


As of 2023, consumers in Iowa were able to purchase short-term health plans, with seven insurers approved to sell the plans in Iowa.6

Frequently asked questions about Iowa Medicaid eligibility and enrollment
How do I apply for Medicaid in Iowa?
To apply for Medicaid:
- Create an account and apply online for Medicaid via the Iowa Department of Human Services (DHS) portal. You can also apply through HealthCare.gov
- Print a Medicaid application in English or Spanish. Mail your completed application to Imaging Center 4; PO Box 2027; Cedar Rapids, Iowa 52406.
- Get help with your Iowa Medicaid application by calling 1-855-889-7985.
How does Medicaid provide financial help to Medicare beneficiaries in Iowa?
Many Medicare beneficiaries receive help from Medicaid with Medicare premiums, prescription drug expenses, and costs that aren’t covered by Medicare — such as long-term care.
Our guide to financial resources for Medicare enrollees in Iowa includes overviews of those programs, including Medicare Savings Programs, long-term care benefits, and income guidelines for assistance.
How is Iowa handling Medicaid renewals after the pandemic?
As is the case nationwide, enrollment in Medicaid in Iowa has trended upward throughout the COVID pandemic. From March 2020 through March 2023, Medicaid disenrollments have been paused nationwide, in response to the pandemic. This will end on March 31, 2023, however, and states can resume disenrollments as of April 1, 2023, for people who are no longer eligible for Medicaid.
Although disenrollments can resume as of April 1, states have the option to push that date forward a bit. The federal government is allowing states to being the process of returning to normal eligibility redeterminations in February, March, or April of 2023, and renewals are generally a multi-month process. States then have 12 months to initiate eligibility redeterminations for all Medicaid members, and 14 months to complete the process. This timeframe is referred to as “unwinding” of the pandemic-era continuous coverage requirements. Iowa’s Department of Health and Human Services has a comprehensive page devoted to the unwinding, as well as a resource library and an interactive unwinding dashboard. There is also a webinar devoted to explaining how the unwinding process will work in Iowa.
Iowa opted to begin the process in February 2023, starting with passive/automatic renewals when possible. Iowa is prioritizing eligibility redeterminations for people who haven’t had a successful renewal within the past 12 months (many members have had their coverage renewed, either passively or actively, within the past 12 months, even though that wasn’t necessary in order to maintain coverage during the pandemic). So some people will see their normal renewal date change (eg, your renewal date when you first enrolled might have been October, but you might now find that it’s been changed to May because you don’t have an up-to-date renewal in the system and your case is being prioritized for review).
For people who have an April renewal date, Iowa began processing renewals in February 2023. But again, this started with automatic/passive renewals, and members who are renewed this way (based on data the state already has in its system) will just receive a notification that their coverage has been renewed. But people who can’t be automatically renewed received a renewal packet in the mail in late February or early March, with a due date of April 5. If people don’t respond to these packets, or if they do respond and it’s confirmed that they’re no longer eligible, their disenrollments will come at the end of April, meaning that their Medicaid will no longer be in effect starting in May.
This process will repeat each month for the next 12 months (so redeterminations initiated in March will be for people whose renewal date is in May, and terminations for people in that group who are no longer eligible will take effect in June, and so on). As is the case in every state, Iowa Medicaid enrollees need to make sure that their contact information is up-to-date in the Medicaid system, so that they’ll receive renewal packets in a timely manner.
Iowa will have two new Medicaid managed care contracts starting in July 2023, with Amerigroup Iowa and Molina. This will give Medicaid members who are enrolled in managed care an opportunity to switch to a different managed care organization, but this is unrelated to the unwinding process. So it’s important for Iowa Medicaid members to understand that they may be receiving communications about both the unwinding/redeterminations as well as the opportunity to select a new managed care organization, if applicable (more details below about Iowa’s Medicaid managed care program and its history).
Legislation impacting Iowa Medicaid
Does Iowa have a Medicaid work requirement?
No. Lawmakers in Iowa still considered a Medicaid work requirement during the 2020 legislative session (SF2366), and although it passed in the Iowa Senate, it did not advance in the House. Under the Trump administration, 1115 waivers to implement work requirements were approved for several states. But the COVID pandemic essentially put an end to Medicaid work requirements and all of the approvals were ultimately revoked by the Biden administration.
Medicaid eligibility expansion in Iowa – with a waiver
The federal government laid out very specific parameters for Medicaid expansion under the ACA. But states have the option of seeking a waiver from CMS in order to implement unique approaches to Medicaid expansion, and still receive federal funding to do so.
In December 2013, Iowa received a waiver for its alternative to the ACA’s Medicaid expansion. Under a program called the Iowa Health and Wellness Plan (IHAWP), very low-income residents (household income at or below the poverty level) would be enrolled in a state-run health plan (Iowa Wellness Plan, or IWP) and, in some cases, be required to pay modest premiums. Other residents with slightly higher incomes (101% to 138% of the federal poverty level) would purchase insurance through the marketplace via a program called the Iowa Marketplace Choice Plan (MPC), with premiums paid by the federal government.
The federal government approved two waiver amendments in December 2014. One allowed Iowa to continue not providing non-emergency transportation. The other allowed Iowa to continue charging a monthly premium for beneficiaries with income under 138% FPL. Beneficiaries could reduce or eliminate the premium if they completed a wellness exam and health risk assessment.
The Iowa Health and Wellness Plan launched Jan. 1, 2014, and about 120,000 people were enrolled as of late December 2014 (50% more than the 81,000 people the state had projected). But problems began to crop up early on.
Only Coventry and CoOpportunity Health (an ACA-created CO-OP) participated in the privatized Medicaid program (MPC) in Iowa, and CoOpportunity was liquidated by state regulators at the beginning of 2015. Around the same time, Coventry told state regulators that it was experiencing financial hardships as a result of covering MPC members, and was considering dropping out of the program. By June 2015, just 6,937 IHAWP members were enrolled in Coventry plans; the remaining 127,016 were covered by IWP, including more than 33,500 people who would have otherwise been eligible for a private plan under MPC — there were simply no private carriers available to provide coverage.
Medicaid eligibility expansion in Iowa— without a waiver, but with managed care
In July 2015, Iowa officials announced that they were abandoning their Medicaid demonstration waiver, and would instead implement Medicaid expansion as called for in the ACA, but with a Medicaid Modernization managed care waiver instead, switching Iowa Medicaid enrollees to a Medicaid managed care system (39 states and DC already had Medicaid managed care programs).
Eligibility for coverage under Iowa’s Medicaid expansion was unchanged in the transition; Medicaid coverage continued to be available to Iowa residents with household incomes up to 138% of the poverty level. But enrollees with incomes between 101% and 138% of the poverty level were no longer enrolled in private exchange plans as of 2016. Instead, they are enrolled in a private Medicaid managed care program, just like the rest of the Medicaid population in Iowa.
560,000 Iowa Medicaid beneficiaries were scheduled to transition to the Medicaid managed care system (Iowa Health Link) as of January 1, 2016. The Medicaid enrollees were supposed to select a managed care program by mid-December, but many enrollees were having trouble determining which managed care programs included their doctors and hospitals. As a result, the federal government delayed Iowa’s switch to Medicaid managed care until March 1, 2016. The federal government ultimately gave the go-ahead for the switch on February 23, but added an extra month to allow enrollees, MCO carriers, and providers time to make the change. The Medicaid managed care system in Iowa took effect April 1, 2016.
In August 2015, Iowa officials announced that Medicaid managed care contracts would be awarded to four private carriers in 2016: AmeriHealth Caritas, Anthem (Amerigroup), UnitedHealthcare, and WellCare. Seven other carriers bid on the contracts but were not selected. But in December, WellCare lost their contract “due to issues in the bidding process,” and the number of participating managed care providers dropped to three. People who had already enrolled in WellCare’s program were transitioned to one of the other three managed care programs.
In January 2016, questions arose about the business practices of AmeriHealth and UnitedHealthcare in Medicaid managed care programs in other states, including neighboring Kansas. The carriers had allegedly been denying claims for Medicaid patients in an effort to curtail costs, and had to pay tens of thousands of dollars in settlements with the states involved. However, the carriers’ contracts for Iowa’s Medicaid managed care program remained on-track, and AmeriHealth Caritas Iowa, Amerigroup, and UnitedHealthcare were all participating in the MCO program when it launched.
Transition in Iowa to Medicaid managed care in 2016, and subsequent shifts in insurer participation
Iowa opted to switch the entire Medicaid program to managed care, intending to make the switch as of January 1, 2016. The federal government determined in December 2015 that Iowa needed additional time to make the transition to Medicaid managed care, and the new system, dubbed Iowa Health Link, took effect April 1, 2016. Patients and providers reported a fairly rocky switch to the privatized Medicaid system.
Democrats in the Iowa Senate tried to halt the switch to managed care, and passed Senate File 2125 in February 2016, which would have terminated the managed care contracts and instructed the existing Medicaid fee-for-service program to focus on improving patient outcomes and access to care, and increasing efficiency (the bill did not advance further, however).
There were initially three insurers offering Medicaid managed care through Iowa Health Link: Amerigroup, AmeriHealth Caritas, and UnitedHealthcare. But Iowa and AmeriHealth Caritas were unable to agree on the terms of a contract renewal in late 2017, and AmeriHealth Caritas withdrew from Iowa Health Link at the end of November, 2017, when their contract ended. And around the same time, Amerigroup informed the state that they did not have the capacity to accept new members.
So 200,000 AmeriHealth Caritas members were transitioned to UnitedHealthcare, which was the only Iowa Health Link insurer accepting new Medicaid enrollees. There were another 10,000 AmeriHealth Caritas members who had selected AmeriGroup as their new Medicaid managed care plan before Amerigroup closed new enrollments, and the state transitioned those individuals temporarily to Medicaid fee for service (ie, not managed care).
The state continued to work with Amerigroup to solve the capacity issue, and by early 2018, Amerigroup had opened up its program to new Iowa Medicaid enrollees once again. The people who had selected Amerigroup in the fall of 2017 and had instead been enrolled in fee-for-service Medicaid were covered under Amerigroup as of March 1, 2018. And new Iowa Health Link members whose coverage started May 1, 2018 or later were able to select from UnitedHealthcare or Amerigroup.
But UnitedHealthcare exited the program in mid-2019 and was replaced by Iowa Total Care. As of 2020, Iowa Medicaid enrollees could choose a plan from Amerigroup Iowa or Iowa Total Care, although the state withheld funding from Iowa Total Care in early 2020 due to incorrect payments and faulty record-keeping.
By 2022, new contracts had been awarded for Iowa’s Medicaid managed care program, with three carriers that will be participating in the program as of July 2023: Centene/Iowa Total Care (existing contract runs through 2025), Molina (new contract), and Elevance/Amerigroup Iowa (new contract). The state is working to ensure that problems that occurred during previous managed care transitions are not repeated.
More information about the Iowa Medicaid program
Iowa implemented its Medicaid program in July 1967. Iowa Medicaid Enterprise (IME), a division of the Iowa Department of Human Services (DHS), is the name of the entity that administers the state’s Medicaid program.
Total enrollment in Iowa’s Medicaid program was 874,481 as of December 2022. Enrollment has increased by about 77% since the first ACA open enrollment period began in the fall of 2013. Iowa Medicaid has served as a safety net during the Covid-19 months, with enrollment increasing significantly since early 2020 (as has been the case nationwide).
Footnotes
- “October 2023 Medicaid & CHIP Enrollment Data Highlights” , Medicaid.gov, Accessed February 2024 ⤶
- “Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment”, KFF.org, Accessed February 2024 ⤶ ⤶
- “Unwind Resource Library” , hhs.iowa.gov, Accessed February 2024 ⤶
- “Iowa dental insurance guide 2023” healthinsurance.org, Accessed September 2023 ⤶
- “Medicare Monthly Enrollment”</a> CMS.gov, April 2023 ⤶
- “Availability of short-term health insurance in Iowa” healthinsurance.org, Sept. 5, 2023 ⤶

