Medicaid eligibility and enrollment in Oregon
Temporary further expansion of Medicaid to 200% FPL for those who would otherwise lose coverage during “unwinding” of continuous coverage rule


Who is eligible for Medicaid in Oregon?
Medicaid in Oregon is called Oregon Health Plan. Coverage is available to the following populations:
- Adults under 65 with household incomes up to 138% of the federal poverty level (for those who were already enrolled in Medicaid prior to the end of the COVID-related continuous coverage rule, eligibility has been temporarily extended to 200% of the poverty level)
- Pregnant women and infants with household incomes up to 185% of poverty.
- Children under age 19 with household incomes up to 305% of poverty, regardless of immigration status. (Children are allowed to stay enrolled until they turn 6, even if they were to have a change in circumstances that would otherwise cause them to lose eligibility. Children six and older get two years of continuous eligibility, even if circumstances change.)
- The Oregon Breast and Cervical Cancer program is available to women with household income up to 250% of federal poverty level and who are less than 65 years old.
- “youth with special health care needs,” aged 19 to 26, with household income up to 300% of poverty.
for 2026 coverage
0.0%
of Federal Poverty Level
Apply for Medicaid in Oregon
Online at HealthCare.gov or by phone at 800-318-2596. If you're pregnant, a tribal member, a refugee, or have other special eligibility status, you can apply through OregonHealthCare.gov.
Eligibility: The aged, blind, and disabled. Also, coverage is available if your household income does not exceed 138% of poverty (185% for pregnant women and infants) and CHIP is available for children with household incomes up to 300% of poverty.
ACA’s Medicaid eligibility expansion in Oregon
Oregon was far ahead of the pack on Medicaid expansion and reform. The state expanded Medicaid (Oregon Health Plan) to cover people with incomes up to the poverty level in 1994. Budget woes resulted in benefits being scaled back over the years and enrollment was suspended from 2004 to 2008.
But when the Affordable Care Act (ACA) offered states the opportunity to expand Medicaid to everyone with incomes up to 133% of poverty (138% with the built-in income disregard), it was an obvious choice for Oregon’s legislature and governor, particularly given the fact that the federal government paid the full cost of expansion through 2016, and will always pay at least 90% of the cost of covering the expansion population.
By May 2023, enrollment in Oregon Health Plan stood at more than 1.5 million people. This was an increase of more than 33% since March 2020, when the federal Families First Coronavirus Response Act was enacted. That legislation provided states with additional federal Medicaid funding during the pandemic (phasing out during 2023), but also prevented states from disenrolling people from Medicaid during the pandemic (that rule ended March 31, 2023).
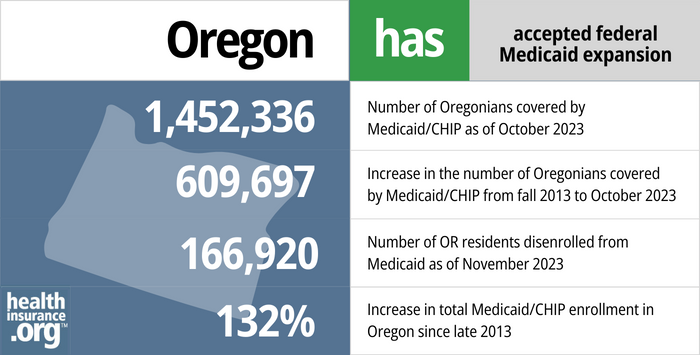
- 1,452,336 – Number of Oregonians covered by Medicaid/CHIP as of October 20231
- 609,697 – Increase in the number of Oregonians covered by Medicaid/CHIP from fall 2013 to October 20232
- 166,920 – Number of OR residents disenrolled from Medicaid as of January 20243
- 132% – Increase in total Medicaid/CHIP enrollment in Oregon since late 20132
Explore our other comprehensive guides to coverage in Oregon

We’ve created this guide to help you understand the Oregon health insurance options available to you and your family, and to help you select the coverage that will best fit your needs and budget.


In 2023, six insurers offer stand-alone individual/family dental coverage through the health insurance Marketplace in Oregon.


As of April 2023, more than 920,000 people in Oregon have Medicare coverage.4 Learn more about enrollment in Medicare and the state’s protections for Medigap enrollees.


Duration of short-term health insurance plans in Oregon is restricted to three months. As of 2023, at least three insurers offer short-term health insurance plans in Oregon.

Frequently asked questions about Oregon Medicaid
How do I apply for Medicaid in Oregon?
If you are under 65 and don’t have Medicare:
- The best way to enroll in Oregon Health Plan is online at HealthCare.gov or One Oregon.
- You can also contact HealthCare.gov by phone to enroll at 1-800-318-2596.
- Residents with certain special-eligibility status can enroll through Oregonhealthcare.gov.
- You can also get in-person assistance with an application by contacting a community partner. This link will help you find assistance in your area.
- Those who are currently enrolled Oregon Health Plan and Healthy Kids need to renew their benefits annually. They will receive a notice from the state when it’s time to do this, and the Oregon Health Plan website has renewal forms and full renewal applications available for existing members.
If you are 65 or older or have Medicare:
- You can apply for Medicaid or a Medicare Savings Program (MSP) using One Oregon.
- You can also receive free assistance with applying through an Area Agency on Aging (AAA) or a Department of Human Services Office for Aging and People with Disabilities.
How does Medicaid provide financial assistance to Medicare beneficiaries in Oregon?
Many Medicare beneficiaries receive Medicaid’s help with paying for Medicare premiums, affording prescription drug costs, and covering expenses not reimbursed by Medicare – such as long-term care.
Our guide to financial assistance for Medicare enrollees in Oregon includes overviews of these benefits, including Medicare Savings Programs, long-term care coverage, and eligibility guidelines for assistance.
Legislation impacting Oregon Medicaid
Oregon received federal approval to temporarily further expand Medicaid as a “bridge” program until BHP is established
Oregon is working to create a Basic Health Program, which will cover people with income between 138% and 200% of the poverty level. But Oregon has also temporarily further expanded Medicaid, up to 200% of the poverty level, to adults who were enrolled under Medicaid expansion during the pandemic.
Until the BHP is up and running (expected to be the summer of 2024), this unique approach helps to prevent coverage losses during the “unwinding” of the COVID-related continuous coverage rule. Without the temporary additional Medicaid expansion, the state estimated that 300,000 people would have lost coverage during the unwinding period. But that number will be lower now that the state is temporarily allowing adult Medicaid enrollees to continue to be covered by Oregon Health Plan with income as high as 200% of the poverty level.
Oregon’s approach, (via an approved amendment to an existing 1115 waiver) temporarily allows people age 19-64 to stay on Medicaid if their income isn’t more than 200% of the poverty level, assuming they would otherwise have become ineligible for Medicaid due to their income (ie, their income has risen above 138% of the poverty level, but doesn’t exceed 200%).
In Oregon, Medicaid disenrollments resume at the end of July, or at the end of September for members who don’t respond to their renewal packet.
For people who end up needing to purchase their own replacement coverage (ie, they lose Medicaid and aren’t eligible for Medicare or an employer’s plan), HealthCare.gov is offering an extended enrollment opportunity, from March 31, 2023 through July 31, 2024, for anyone who loses Medicaid at any time during that window. Oregon uses HealthCare.gov as its marketplace/exchange, so this enrollment window will be available to Oregon residents who lose Medicaid during the “unwinding” of the pandemic-related continuous coverage requirement.
New waiver allows for longer continuous eligibility for Oregon Medicaid enrollees
An 1115 waiver, effective October 2022 and valid through September 2027, is allowing Oregon to provide residents with longer stretches of continuous Medicaid coverage. Under the terms of the waiver:
- If a child under age six is determined eligible for Medicaid, they will stay eligible until they turn six, even if their circumstances (family income, etc.) change in a way that would otherwise make them ineligible.
- For people six and older who are determined eligible for Medicaid, they will stay eligible for at least 24 months, even if their circumstances change in a way that would otherwise make them ineligible.
- Young adults (19-26) with special health care needs are eligible for Medicaid with income up to 300% of the poverty level.
Nationwide, Medicaid eligibility was continuous from March 2020 through march 2023, due to the COVID pandemic, although routine eligibility redeterminations resumed in April 2023. And starting in 2024, all states will have to provide at least 12 months of continuous eligibility for children who are determined eligible for Medicaid, even if their circumstances change.
But Oregon’s 1115 waiver allows the state to go well beyond the minimum requirements, ensuring that people maintain continuous coverage and reduce the “churn” that happens when people transition in and out of the Medicaid system due to frequent eligibility changes.
Oregon Medicaid enrollment
Prior to 2014, it was anticipated that Oregon would enroll 400,000 new members in the Medicaid program by 2022. While that prediction may ultimately prove accurate, Medicaid enrollment in Oregon has fluctuated rather dramatically from the launch of the ACA and Medicaid expansion.
In the fall of 2013, prior to the launch of the ACA’s exchanges, Oregon’s total Medicaid/CHIP enrollment stood at more than 626,000.
By March 2016, enrollment in Oregon Medicaid/CHIP was 1,076,961 (a 72% increase compared to 2013 enrollment, which was at that point tied with Colorado for the third highest percentage growth in the country, behind only Kentucky and Nevada).
Then, Oregon Medicaid enrollment dropped sharply from early 2016 to early 2017. Not coincidentally, Oregon had experienced glitches with its Medicaid enrollment platform prior to 2016, and applicants’ eligibility had not been properly screened. Between March 2016 and August 2017, nearly 300,000 enrollees were removed from the Medicaid program once it was determined that they weren’t actually eligible for benefits.
By June 2018, Oregon Medicaid/CHIP enrollment had rebounded to more than 963,000 people. Enrollment grew by more than 100,000 people between then and July 2020, when it reached more than 1,066,000 people. By May 2023, enrollment stood at more than 1.5 million. This was after three years of continuous eligibility for everyone who had been enrolled as of March 2020, when periodic eligibility redeterminations were paused under the federal Families First Coronavirus Response Act.
Fast-track enrollment
Oregon is one of a handful of states that used a fast-track enrollment process prior to 2014 that let them identify Medicaid-eligible residents based on their participation in other state-run programs. Since their income and immigration status were already verified, the people who were identified as fast-track eligible did not have to go through the full application process for Medicaid.
The state sent out notifications to about 300,000 residents, letting them know they were eligible for Medicaid. People who received one of these letters were able to simply fill out the enclosed form and returned it in the postage-paid envelope to be automatically enrolled in Medicaid. Oregon also had a system that let eligible fast-track enrollees complete the enrollment process by telephone.
Oregon Medicaid history
The Oregon Health Plan is Oregon’s Medicaid program, overseen by the Oregon Health Authority. The Oregon Health Plan was conceived and implemented in the late 80s and early 90s. Oregon Medicaid was on the cutting edge of health care reform, addressing the issue of access to healthcare long before most other states.
During that time, physician John Kitzhaber was a state senator and was instrumental in shaping Oregon’s Medicaid program. Kitzhaber went on to be governor of Oregon from 2011 to 2015. During the late 80s/early 90s, Oregon’s uninsured rate was about 18%. According to a Gallup data, that rate had dropped to 14% by mid-2014, and to just 8.8% by mid-2015. That put Oregon third in the nation in terms of percentage drop in the uninsured rate by the first half of 2015.
In 1994, Oregon expanded Medicaid to cover all residents with incomes below the poverty level under a basic benefits package (OHP Standard, as opposed to the OHP Plus program that applies to pregnant women, children, disabled residents, and others who were already eligible for Medicaid). That year, 120,000 newly-eligible residents enrolled, and Portland area hospitals saw a 16% reduction in unpaid medical bills.
In 1995, Medicaid in Oregon began to add mental health and chemical dependency coverage, although these services were removed from the basic benefits package in 2003. In most states, Medicaid was only available to pregnant women, children, seniors, and adults with disabilities prior to 2014 — Oregon was way ahead of its time in expanding basic coverage to everyone living in poverty.
Over the last two decades, Oregon Health Plan has instituted numerous cost-containment measures, including a requirement that limits beneficiaries to a single pharmacy (chosen by the insured member), a disease management program providing case management to clients with specific chronic illnesses, and copays for most adult clients who are not part of exempt groups (tribal members, pregnant women, etc.). Coverage for vision/hearing, and durable medical equipment was eventually discontinued as the state worked to reduce Medicaid expenses.
In addition, the state began requiring small premiums to participate in OHP Standard, and that led to roughly 40,000 enrollees dropping their coverage because they were unable to pay the premiums (now that Medicaid has been expanded, they are once again eligible for coverage without premiums).
By 2004, considerable budget issues led to a ballot initiative that would have generated revenue for OHP via additional income taxes, corporate taxes, and tobacco taxes. The ballot measure failed though, and OHP Standard ceased new enrollments on July 1, 2004. It didn’t open back up again until 2008, at which point there was a lottery to claim 3,000 available spots in the program (tens of thousands of people applied to get one of the spots, and many people applied more than once over the ensuing years).
It was a natural progression for Oregon to accept federal funding to expand Medicaid in 2014. Coverage is now available for all legally present residents with incomes up to 138% of poverty, and the federal government is picking up most of the tab for the newly-eligible enrollees. There’s no longer a lottery system in Oregon — everyone who qualifies can enroll in the program. The Oregon legislature passed an omnibus bill early in 2014 that increased Oregon Health Plan’s budget by $1.17 billion (to a total of $14.4 billion) for 2013 – 2015, in order to get the Medicaid expansion program up and running.
Footnotes
- “October 2023 Medicaid & CHIP Enrollment Data Highlights”, Medicaid.gov, Accessed November 2023 ⤶
- “Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment”, KFF.org, Accessed November 2023 ⤶ ⤶
- ”Medical Redeterminations Dashboard”, Oregon Department of Human Services, Accessed November 2023 ⤶
- “Medicare Monthly Enrollment” CMS.gov, April 2023 ⤶

