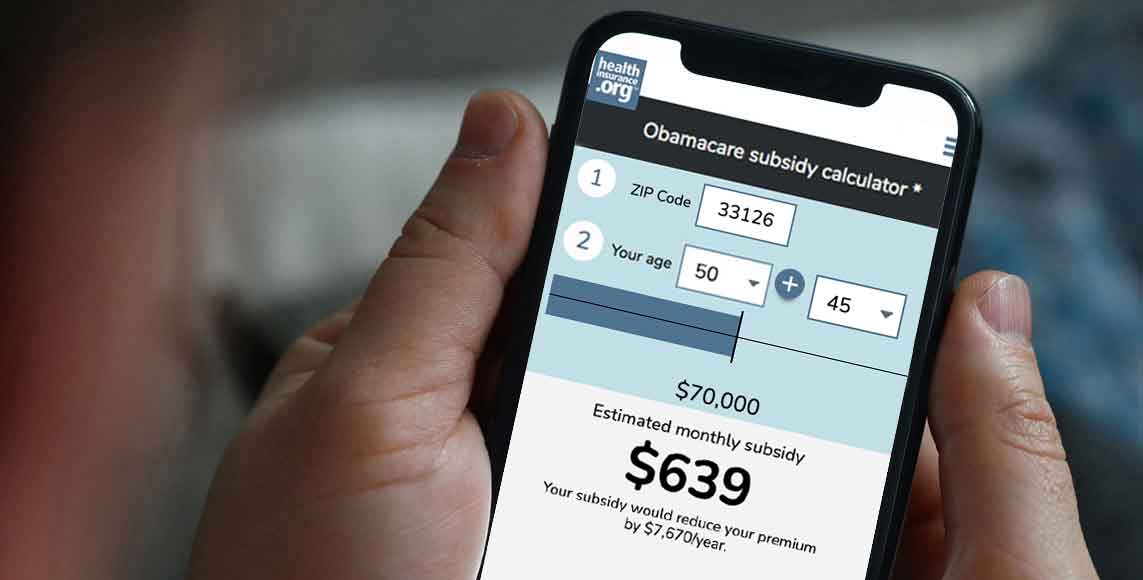
Please provide your zip code to see plans in your area.
Featured

Featured

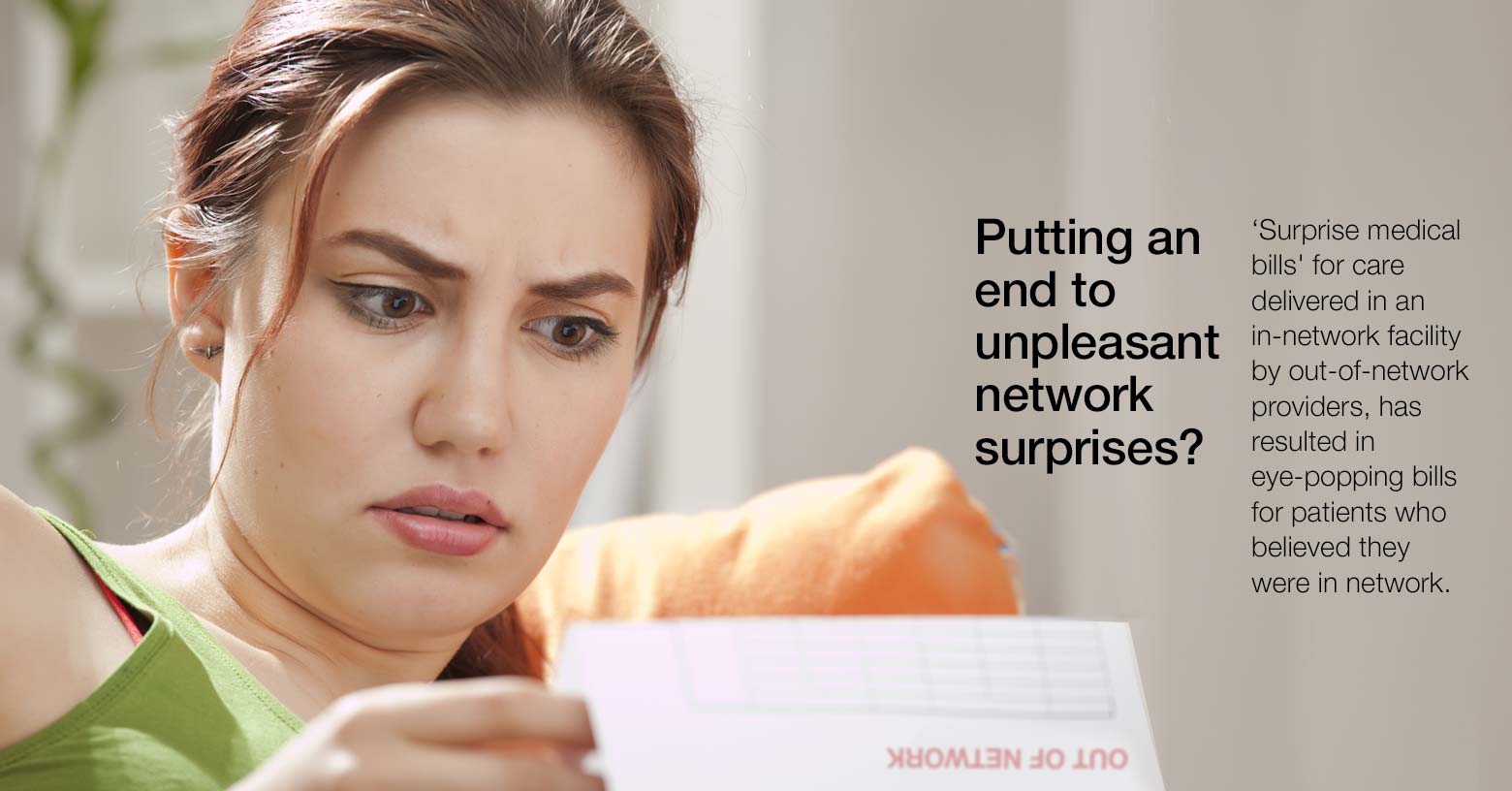
in-network
What does in-network mean?
In network refers to providers or health care facilities that are part of a health plan’s network of providers with which it has negotiated a discount. Insured individuals usually pay less when using an in-network provider, because those networks provide services at lower cost to the insurance companies with which they have contracts. The provider’s contract with the insurer requires the insurer to accept the insurer’s payment (plus the patient’s cost-sharing, such as the deductible, copay, or coinsurance) as payment in full — an in-network provider cannot balance bill a patient.
Some health plans only pay for services when the member uses in-network providers, while other health plans will pay at least some of the claim even if the member uses an out-of-network provider.
Related articles
Signing up for coverage today doesn't mean your coverage will be effective immediately. Here's what you need to know to get coverage in place ASAP.
Insurance industry, healthcare leaders, coverage advocates work with regulators to address consumer concerns about provider networks.
Sweeping health reform legislation delivered a long list of provisions focused on health insurance affordability, consumer protections.
Four designations of managed care affect your healthcare costs and plan benefits – including which medical providers you can access.