Medicaid eligibility and enrollment in Colorado
More than half a million Coloradans are covered under Medicaid expansion; Low-income undocumented pregnant people and children will gain eligibility as of 2025


Who is eligible for Medicaid in Colorado?
Since 2016, Colorado Medicaid has been called Health First Colorado. Colorado’s income limits for Medicaid eligibility are:
- Children up to age 18: Up to 147% of FPL to qualify for Medicaid
- Children up to age 18 who aren’t eligible for Medicaid can qualify for Child Health Plan Plus (CHP+; Colorado’s CHIP coverage) with household income up to 265% of FPL.
- Coverage is available to lawfully-present immigrant children. As of 2025, income-eligible children who are undocumented immigrants will also be eligible for Medicaid/CHP+.
- Pregnant women: Up to 200% of FPL to qualify for Medicaid. Coverage for pregnant women continues for a year after the birth
- Pregnant women who don’t qualify for Medicaid can qualify for CHP+ with family income up to 265% of FPL
- Coverage is available to lawfully present immigrants who are pregnant. As of 2025, this coverage will also be available to undocumented pregnant people who would otherwise qualify for Medicaid/CHP+ except for their immigration status;
- Adults under the age of 65 can enroll in Health First Colorado with household income up to 138% of FPL (this is Medicaid expansion under the ACA)
Note that “income” refers to an ACA-specific version of modified adjusted gross income (MAGI). All of the above income limits include a 5% income disregard that’s added to MAGI for the purposes of determining Medicaid/CHIP eligibility for children, pregnant women, and nonelderly adults.
for 2026 coverage
0.0%
of Federal Poverty Level
Apply for Medicaid in Colorado
Pregnant women, as well as children from birth through age 18 with family income levels up to 265% of FPL; Nonelderly adults — with or without dependent children — with incomes up to 138% of FPL.
Eligibility: Children 0-18 with family incomes up to 147% of FPL; children with family incomes up to 265% of FPL qualify for Child Health Plan Plus (CHP+); pregnant women with family income up to 200% of FPL; (pregnant women with family income up to 265% of FPL qualify for CHP+); non-elderly adults with family income up to 138% of FPL; some individuals who are elderly or disabled.
ACA Medicaid eligibility expansion in Colorado
One of the Affordable Care Act’s primary strategies for reducing the uninsured rate is Medicaid expansion to cover low-income adults under the age of 65. (Eligibility rules did not change for adults age 65 or older; they are still subject to both income and asset limits for Medicaid eligibility. Here’s how that works in Colorado.)
Then-Governor John Hickenlooper signed the legislation authorizing Medicaid expansion in May 2013. As of 2022, Medicaid expansion (Group VIII) enrollment in Colorado was 547,571, accounting for more than a third of the state’s total Medicaid enrollment.
Medicaid enrollment in Colorado grew by 72% in the first two years of Medicaid expansion implementation. Medicaid enrollment growth had largely leveled off by 2016/2017, but it spiked again in 2020, due to the COVID pandemic, and has continued to grow every since, due to the pandemic-related rule that prevented states from disenrolling Medicaid members between March 2020 and March 2023.
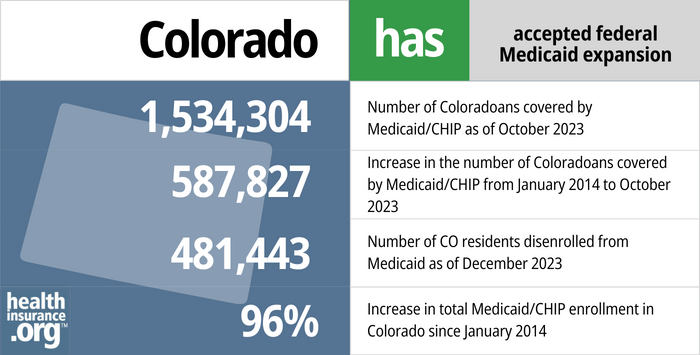
- 1,534,304 – Number of Coloradoans covered by Medicaid/CHIP as of October 20231
- 587,827 – Increase in the number of Coloradoans covered by Medicaid/CHIP from January 2014 to October 20232
- 481,443 – Number of CO residents disenrolled from Medicaid as of December 20233
- 96% – Increase in total Medicaid/CHIP enrollment in Colorado since January 20142
Explore our other comprehensive guides to coverage in Colorado

This guide is designed to help you understand your Colorado health insurance options and possible financial assistance available to you and your family — including federal subsidies and Colorado’s state-funded subsidies.


Want to improve your smile and save some money when you visit the dentist? Our guide explains dental coverage options in Colorado.


More than 1 million Colorado residents were enrolled in Medicare as of May 2023.4 Our Colorado Medicare guide explains the various parts of Medicare, coverage options under Medicare Advantage and Part D, and Colorado regulations regarding Medigap (Medicare Supplement) availability.


Colorado tightened its rules for short-term health plans in 2019.5 The result was that insurers opted to stop selling short-term policies in the state. So although short-term health plans are technically allowed in Colorado, none have been for sale in the state for several years.

Frequently asked questions about Colorado Medicaid eligibility and enrollment
How do I enroll in Medicaid in Colorado?
If you think you may qualify for Health First Colorado Medicaid, you can apply a number of ways:
- Online at Colorado PEAK. (PEAK stands for Program Eligibility and Application Kit.) Colorado PEAK is a website for applying for food, cash, and medical assistance programs. Colorado’s state-run health insurance exchange (Connect for Health Colorado) connects with PEAK, so you’ll be able to enroll in Medicaid or CHIP if you start at the exchange website, too.
- In person at your county office.
- By telephone: 1-800-221-3943 (TDD: 1-800-659-2656).
- By mail: print an application, fill it out, and mail it to the address included on the application form. You can also get a form at your county office or an application assistance site.
How does Medicaid provide financial assistance to Medicare beneficiaries in Colorado?
Many Medicare beneficiaries receive Medicaid financial assistance that can help them with Medicare premiums, lower prescription drug costs, and pay for expenses not covered by Medicare – including long-term care.
Our guide to financial assistance for Medicare enrollees in Colorado includes overviews of these programs, including Medicaid nursing home benefits, Extra Help, and eligibility guidelines for assistance.
How is Colorado handling Medicaid renewals after the pandemic?
As is the case in every state, Medicaid disenrollments were paused in Colorado from March 2020 through March 2023. The continuous coverage requirement was initially slated to last throughout the COVID public health emergency, which ended nationwide on May 11, 2023. But the federal spending bill enacted in late 2022 gave states a firm deadline: The Medicaid continuous coverage requirement ended March 31, 2023, and disenrollments for people who are no longer eligible could resume as early as April 1, 2023.
Health First Colorado (Colorado Medicaid) officials hosted a webinar in January 2023, outlining their plans for the resumption of regular eligibility redeterminations and disenrollments. Another webinar was held in April, and additional webinars will be held quarterly throughout 2023. The state began the first round of eligibility redeterminations in mid-March 2023, sending renewal packets to enrollees whose coverage is due to renew in May. The first round of coverage terminations (for people who are no longer eligible or who don’t respond to the state’s request for eligibility verification) will be on May 31, so June will be the first month that people no longer have Medicaid coverage as a result of the end of the pandemic-related continuous coverage requirements.
Colorado officials have noted that they plan to keep each enrollee’s existing renewal date, so a person whose coverage is due for renewal in October will not get a renewal packet until August, and their coverage will continue until October even if they’re no longer eligible for Health First Colorado. Enrollees can visit this webpage to find out when their renewal date is.
Colorado had about 1.7 million people enrolled in Medicaid/CHIP (CHP+) as of early 2023. Of those enrollees, approximately 768,000 are enrolled due to the continuous coverage requirement, which means that the state either has information indicating that they’re no longer eligible, or the state has not been able to verify their ongoing eligibility. Colorado Medicaid officials estimate that approximately 315,000 people will no longer be eligible for Medicaid and will be disenrolled once the pandemic-related continuous coverage requirements end. But those disenrollments will be spread out over 12 months; some people will not receive their renewal packet until late 2023 or early 2024.
Starting in January 2023, Colorado Medicaid’s renewal packets (which have been sent out throughout the pandemic, although people could ignore them and still keep their coverage) have red lettering on the front of the envelope that says “URGENT – PLEASE REPLY” in an effort to get enrollees’ attention. The state is also encouraging all Medicaid enrollees to make sure that their contact information is updated and to promptly reply to any request for information that they receive from the Medicaid agency. In April, the state noted that they have been able to update contact information for about 70% of their returned mail cases (ie, where the state initially had an outdated address on file and notices sent to that address were returned as undeliverable).
Colorado’s Medicaid office and state-run exchange (Connect for Health Colorado) have an interoperable system, and plan to work together to get people who are no longer eligible for Medicaid transitioned over to a health plan through the exchange, unless they have access to coverage from an employer or Medicare. And Colorado’s Division of Insurance has confirmed that a person who enrolled in Medicare but didn’t sign up for a Medigap plan because they were also able to keep their Medicaid during the pandemic, will have a six-month window with guaranteed-issue access to Medigap plans after their Medicaid terminates.
Legislation impacting Colorado Medicaid
Medicaid expanded to cover undocumented pregnant people as of 2025
In June 2022, Colorado Gov. Jared Polis signed HB1289 into law (details here). Under the terms of the new law, Medicaid and CHIP coverage will be available, starting in 2025, to undocumented pregnant people and children who would otherwise be eligible except for their immigration status.
Colorado was already one of the states that provided Medicaid/CHIP coverage to lawfully present immigrant children and pregnant women who hadn’t yet been in the U.S. for five years (there is normally a five-year wait before a lawfully present immigrant can obtain Medicaid or CHIP, but states can opt to waive that waiting period).
But starting in 2025, Colorado will join several other states that are using state funds to provide Medicaid/CHIP coverage to undocumented children and undocumented pregnant people who would otherwise qualify based on their income. And postpartum Medicaid coverage will continue for a year after the baby is born, helping to improve maternal health in Colorado.
Colorado Medicaid history
The federal legislation establishes Medicaid was enacted in 1965, and Colorado authorized its program in 1969. Milestones in Colorado’s Medicaid and Child CHP+ programs, as well as federal Medicaid legislation, are detailed on the Colorado Center on Law & Policy website.
Medicaid expansion in Colorado went into effect Jan. 1, 2014, and Colorado Medicaid enrollment has grown by 118% in the ensuing years. The growth includes both those who were newly eligible under Medicaid expansion as well those who qualified under existing eligibility criteria but had not previously enrolled.
The Trump administration began approving work requirements for Medicaid programs in early 2018. But Medicaid work requirements are not in effect anywhere in the country as of 2021, due to court rulings, state decisions to suspend them, and the COVID pandemic. And the Biden administration has revoked all previously-approved Medicaid work requirement waivers. But in the early days of work requirement proposals, numerous Republican governors expressed an interest in them, as did a few Democrats.
Colorado expanded Medicaid as called for in the ACA, with no state-based changes to the program. But in February 2018, Democratic Gov. John Hickenlooper, noted that he would be open to the possibility of imposing a Medicaid work requirement in an effort to prevent people from “freeloading on the system.” S.B.214, introduced the following month, would have directed the state to seek permission from CMS to implement a Medicaid work requirement, a monthly income verification requirement, and a five-year limit on Medicaid coverage for non-disabled enrollees. But the bill died ten days later, in a 3-2 vote in the Health and Human Services Committee.
Hickenlooper was term-limited as governor, and now represents Colorado in the U.S. Senate. Jared Polis was elected as Colorado’s governor in 2018 and took office in January 2019. Polis is on record as opposing Medicaid work requirements.
Footnotes
- “September 2023 Medicaid & CHIP Enrollment Data Highlights” , Medicaid.gov, Accessed February 2024 ⤶
- “Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment”, KFF.org, Accessed February 2024 ⤶ ⤶
- “Continuous Coverage Unwind Reports” , hcpf.colorado.gov, Accessed January 2024 ⤶
- “Medicare Monthly Enrollment” CMS.gov, May 2023 ⤶
- “Code of Colorado Regulations eDocket” Colorado Secretary of State, accessed August 2023 ⤶

