Medicaid eligibility and enrollment in Louisiana
Healthy Louisiana, the state’s Medicaid expansion program, covers 773,000 low-income adults as of 2023


Who is eligible for Medicaid in Louisiana?
Depending on the reason for eligibility, low-income Louisiana residents can qualify for Medicaid based on income alone, or a combination of income and assets. Eligibility is based only on household income for children, people who are pregnant or postpartum (this now extends for a year after the baby’s birth), and adults up to age 64 (income limits are different for each of those groups). But for the aged, blind, and disabled, eligibility rules are more stringent, with both income limits and asset limits.
Learn how states that expanded Medicaid might reduce spending on Medicaid.
For the groups that qualify based on income alone, eligibility is determined as a percentage of the federal poverty level (FPL). You can see 2023 FPL numbers here; the federal government updates FPL numbers in January, and Louisiana begins to use them for Medicaid eligibility starting in March. The following income limits are used to determine Medicaid eligibility in Louisiana (these numbers include a built-in 5% income disregard that’s used for income-based Medicaid eligibility determinations):
- Children ages 0-18: 217% of the federal poverty level (FPL);
- Children with family income between 218% and 255% of FPL are eligible for the Louisiana Children’s Health Insurance Program (LaCHIP)
- Adults under the age of 65: 138% of the federal poverty level (the state has a page that lists this in weekly and monthly income amounts for 2023). Note that this income limit is also applicable for pregnant women; many states have higher Medicaid thresholds for people who are pregnant, but Louisiana does not. (Percentage of poverty income limits are the same for a pregnant woman or a woman who is not pregnant, but a pregnant woman counts as two people for Medicaid eligibility determination, as is the case nationwide.)
Individuals who receive Supplemental Security Income (SSI) — who are elderly, blind or disabled — or who meet certain other income and asset guidelines can also qualify for Medicaid.
for 2026 coverage
0.0%
of Federal Poverty Level
Apply for Medicaid in Louisiana
You can apply at the Louisiana Medicaid Online Application Center. Apply by phone at 1-888-342-6207. Apply in person at a Medicaid application center, or fill out a paper application.
Eligibility: Children ages 0-18 with household income up to 212% of FPL; kids with family income between 212-250% of FPL are eligible for the Louisiana Children’s Health Insurance Program. Pregnant women with household income up to 138% of FPL. Parents with dependent children with household income up to 19% of FPL. Visit Louisiana.gov for those who receive SSI or who are elderly, blind or disabled.
When did Louisiana expand Medicaid?
Louisiana’s Medicaid expansion program, called Healthy Louisiana, took effect on June 1, 2016. Earlier that year, on January 12, 2016, newly inaugurated Governor John Bel Edwards signed his first executive order to start the process of Medicaid expansion in Louisiana. Edwards had taken office the day before, and followed through on his promise that Medicaid expansion would be one of his first actions as governor.
Prior to June 1, 2016, Medicaid eligibility for adults in Louisiana was unchanged from 2013, and childless adults were ineligible for coverage, regardless of how low their incomes were. That created a coverage gap, since people with income below the poverty level cannot obtain subsidies in the exchange, so they had no realistic access to health coverage until Medicaid was expanded.
About 105,000 of the people who were newly eligible for Healthy Louisiana were expected to be auto-enrolled under a program the state used to identify eligible residents based on their participation in SNAP (Supplemental Nutrition Assistance Program, often referred to as food stamps). Several states already used similar auto-enrollment programs, but only for initial Medicaid enrollment. Louisiana was the first state in the nation to gain HHS approval to use SNAP enrollment to automate the initial Medicaid enrollment process as well as the annual renewal.
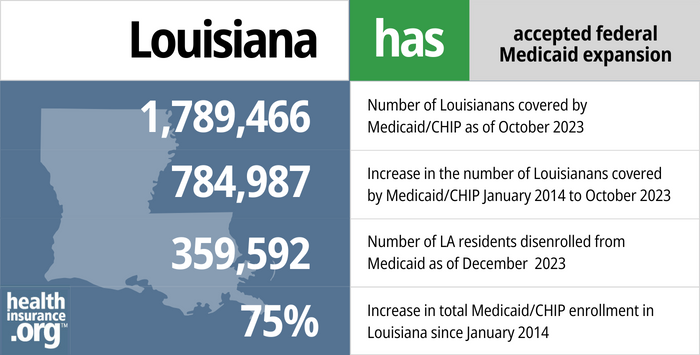
- 1,789,466 — Number of Louisianans covered by Medicaid/CHIP as of October 20231
- 784,987 — Increase in the number of Louisianans covered by Medicaid/CHIP from January 2014 to October 20232
- 359,592 — Number of LA residents disenrolled from Medicaid as of December 20233
- 75% — Increase in total Medicaid/CHIP enrollment in Louisiana since January 20142
Explore our other comprehensive guides to coverage in Louisiana

This guide was created to help make it easier to choose the right health insurance for yourself and your family. A plan from the Affordable Care Act (ACA) Marketplace may be a good choice for many people.


Dental plans in Louisiana cost an average of $41 per month in 2022.4 Compare options to find the right dental plan.


Use our guide to help you understand Medicare Parts A, B, C, and D, along with Medicare supplement (Medigap) plans. Learn more about Medicare regulations in the state.


In Louisiana, short-term health insurance plans can initially last up to 364 days and can be renewed for up to three years. However, a few insurers may have plans with even shorter timeframes and may not allow renewals.5

Frequently asked questions about Louisiana Medicaid eligibility and enrollment
How do enroll in Medicaid in Louisiana?
There are several options for applying for Medicaid if you are under 65 (and don’t also have Medicare).
- You can apply online through the Louisiana Medicaid Online Application Center or at Healthcare.gov.
- You can apply over the phone, toll-free. The number is 1-888-342-6207.
- You can apply in person at a Medicaid application center.
- You can apply by mail or fax. Fill out the application and then mail it to Medicaid; P.O. Box 91278;
Baton Rouge, LA 70821-9278; or fax it to 1-877-523-2987.
If you are 65 or older or have Medicare, use this website or call 888-342-6207 to apply for Medicaid.
How does Medicaid provide assistance to Medicare beneficiaries in Louisiana?
Many people with Medicare receive help through Medicaid with Medicare premium costs, prescription drug expenses, and expenses that Medicare doesn’t cover — such as long-term care.
Our guide to financial resources for Medicare enrollees in Louisiana provides an overview of those programs, including Medicare Savings Programs, nursing home benefits, and income guidelines for assistance.
How is Louisiana handling post-pandemic Medicaid renewals?
Prior to the COVID pandemic, states had to recheck enrollees’ eligibility annually, and disenroll people who were no longer eligible or who didn’t respond to a renewal notification. That was paused during the pandemic: From March 2020 through March 2023, states could not disenroll anyone from Medicaid unless they moved out of state, passed away, or requested a disenrollment.
But that rule ended March 31, 2023, and states are once again required to redetermine all enrollees’ eligibility for Medicaid coverage. States have 14 months to complete this “unwinding” of the COVID-related continuous coverage provisions, during which they must redetermine eligibility for everyone enrolled in their Medicaid programs. States had the option to begin the unwinding process in February, March, or April 2023 (disenrollments couldn’t come earlier than April 1).
Louisiana opted to begin the process in April, and their first disenrollments will come at the end of June 2023, meaning that July 2023 will be the first month that any Louisiana Medicaid enrollees will need to have other coverage in place. Renewals will be spread out over a 12-month period, so some enrollees won’t get a renewal notice until late 2023 or early 2024, and their coverage will continue until at least their renewal date. But if they’re no longer eligible or if they fail to respond to a renewal notice, their coverage will end instead of being renewed.
Louisiana began an outreach campaign ahead of the unwinding period, sending “pink letters” to everyone enrolled in Medicaid. If a Louisiana Medicaid enrollee didn’t receive one of these letters by April 1, 2023, it likely means that the state has outdated contact information on file for that person, and it’s vital that they update their contact information as soon as possible.
Up to 350,000 Louisiana Medicaid enrollees are expected to lose their Medicaid coverage during the unwinding period. But they will be able to transition to other coverage, and can have seamless coverage as long as they enroll in the new plan prior to the Medicaid termination date (so that the new plan takes effect the first of the month following disenrollment from Medicaid). Many people will be able to transition to an employer-sponsored plan. Some will be able to transition to Medicare (if they became eligible during the three-year continuous coverage period but didn’t enroll because their Medicaid didn’t terminate). The rest will be able to enroll in a plan through HealthCare.gov, which is the marketplace/exchange platform in Louisiana.
There is an extended special enrollment period during which a person who loses Medicaid can enroll in a plan through HealthCare.gov anytime between March 31, 2023 and July 31, 2024. But again, it’s essential to submit the application prior to the loss of Medicaid coverage if you want to avoid a gap in coverage, as marketplace coverage will not have a retroactive effective date.
How many people are enrolled in expanded Medicaid in Louisiana?
As of March 2023, there were more than 773,000 residents enrolled in Healthy Louisiana, the state’s Medicaid expansion program. That was far more than the roughly 400,000 the state had initially expected, but the COVID pandemic has pushed Medicaid expansion to record highs nationwide, and Medicaid expansion has proven to be a true safety net during the pandemic.
As of early 2022, more than 2 million Louisiana residents — about 40% of the state’s population — were enrolled in Medicaid/CHIP. This includes the Healthy Louisiana population as well as the traditional Medicaid populations, such as the elderly, children, and certain disabled residents.
Legislation impacting Louisiana Medicaid
Has Louisiana extended postpartum Medicaid to 12 months?
Yes, Louisiana’s postpartum Medicaid coverage for new mothers continues for 12 months after the baby is born. In April 2022, CMS announced that Louisiana was utilizing a provision in the American Rescue Plan to extend postpartum Medicaid and CHIP benefits to last 12 months (it had previously ended at 60 days postpartum). CMS noted that 14,000 pregnant and postpartum people in Louisiana were receiving the extended benefit.
Louisiana was the first state to extend postpartum coverage as part of its state plan amendment using American Rescue Plan funding. Three other states (Illinois, New Jersey, and Virginia) had implemented extended postpartum coverage using 1115 waivers the year before. As of 2023, the majority of the states have either incorporated extended postpartum Medicaid coverage into their state plan amendments, or have plans to do so in the near future.
Louisiana is fairly unique, however, in terms of how low its income limit is for pregnant women to qualify for Medicaid, at 138% of the poverty level. Only three other states (Idaho, Oklahoma, and South Dakota) have an income limit this low. Since Louisiana has expanded Medicaid under the ACA, all adults under the age of 65 are also eligible for Medicaid with household income up to 138% of the poverty level.
So in Louisiana, LaMOMS coverage (for pregnant women) has the same income limits as Healthy Louisiana (Medicaid expansion, for adults under age 65). But the primary difference is that a pregnant woman counts as two people when Medicaid eligibility is determined (this is true nationwide). So if a woman is part of a household of two and then becomes pregnant, she’s then considered part of a household of three, which means the household income level can be as high as $2,895 per month in 2023 and she’ll qualify for Medicaid (without being pregnant, as part of a household of two, the household income would have to be no more than $2,268 for the adults in that household to qualify for Healthy Louisiana).
New Medicaid eligibility and enrollment system launched in November 2018
In November 2018, Louisiana rolled out a new Medicaid eligibility and enrollment system that allows for real-time eligibility determinations using data from state and federal systems, instead of relying on manual eligibility determinations. And under the new system, enrollees would no longer receive phone calls from Louisiana Medicaid when their coverage is up for renewal; notices and requests for additional information would be sent by mail instead, and the system was set up to require enrollees to provide updated information in a timely manner in order to avoid termination of their coverage.
However, in August 2019, the state temporarily suspended the program that would terminate Medicaid coverage for people who don’t respond to requests for updated information. And as described above, Medicaid disenrollments were paused nationwide from March 2020 through March 2023, due to the COVID pandemic. The new system that Louisiana implemented in 2018 automatically connects to state and federal databases to obtain member information regarding income and other eligibility requirements, and that will once again be in use after the PHE ends.
Louisiana enacted legislation in 2018 to create a workforce training program
H.B.735, which passed 97-1 in the House and 32-0 in the Senate, was signed into law in May and took effect in August 2018. The law directs the state to create a workforce training and education pilot program for “improving employment opportunities and promoting workforce advancement” among people receiving public assistance, including Medicaid. The pilot program debuted in 2019 in Monroe, with voluntary enrollment. Enrollees receive assistance with job training, job referral, career planning, apprenticeships and other job skills development.
The long path to Medicaid expansion
On November 21, 2015, Democrat John Bel Edwards won the runoff gubernatorial election in Louisiana. Edwards supported Medicaid expansion as called for in the ACA, and his win immediately made Medicaid expansion much more likely in Louisiana. He took action to expand Medicaid on just his second day in office, and the expanded eligibility rules took effect several months later.
Former Governor Bobby Jindal was emphatically opposed to Medicaid expansion, but was not eligible to run in the 2015 gubernatorial race due to term limits. There was a primary election in October 2015, but none of the four candidates received a majority of the vote. So a runoff election was scheduled for November 21, 2015, with voters deciding between the two candidates who garnered the most votes in the first election (Democratic Minority leader of the Louisiana House of Representatives, John Bel Edwards; and Republican Senator David Vitter).
All four of the primary candidates had previously expressed at least some degree of willingness to accept federal funds to expand Medicaid, although all but Edwards had called for using a section 1115 waiver to craft Medicaid expansion in a state-specific way. Edwards’ support for Medicaid expansion was unequivocal.
In addition, lawmakers in Louisiana passed House Concurrent Resolution 75 in June 2015, which helped pave the way for the expansion of Medicaid. HCR75 allowed hospitals to implement a fee that would generate the revenue needed to pay the state’s portion of the cost of expanding Medicaid (the federal government will always pay 90% of the cost, but by 2020, states were responsible for 10% of the cost of covering the expansion population; hospitals tend to support Medicaid expansion, as they face dire budget cuts in states that haven’t expanded coverage). HCR75 gave Edwards until April 1, 2016 to propose a plan to expand Medicaid, but he wasted no time in issuing the Medicaid expansion executive order the day after taking office.
Lawmakers considered a Medicaid work requirement in 2018, but legislation didn’t pass
In early 2018, Louisiana Gov. John Bel Edwards said that his administration was “actively working” on ideas for implementing a “reasonable” work requirement for the state’s Medicaid program. Bel Edwards, a Democrat, was the prime mover in the state’s expansion of Medicaid in 2016.
In 2017, Louisiana enacted S.R.163, which requires the Louisiana Department of Health to provide monthly data to lawmakers on a variety of Medicaid-related metrics, including the total number of Medicaid expansion enrollees and the number of Medicaid expansion enrollees who have earned income.
According to H.B.3, which was introduced in early 2018, the state had reported that as of December 2017, enrollment in Medicaid expansion stood at 453,000 people, and “fewer than 284,000” of those individuals had earned income (even before S.R.163 was enacted, the Louisiana Department of Health had been providing detailed, up-to-date reports about Medicaid expansion enrollment, which are available to the public but do not include data about income or the work status of enrollees).
The Louisiana House passed H.B.3 in March 2018, but the bill did not advance in the Senate. It called for a Medicaid work requirement, but had been amended to ensure that people wouldn’t lose access to Medicaid if they didn’t comply with the work requirement.
S.B.77, which was introduced in the Senate in 2018 but did not progress to a vote, would have directed the state to seek a waiver from CMS, by January 2019, in order to implement a work requirement for Louisiana Medicaid expansion. The work requirement would have applied to people ages 19 to 64, but would have exempted pregnant women and people with disabilities, along with other populations that would have been detailed in the waiver proposal.
H.B.46, which was introduced in the House in 2018 but did not progress to a vote, would also have directed the state to seek a waiver from CMS in order to implement a work requirement for non-disabled adults age 19 to 64 who are enrolled in Medicaid and not caring for a child under the age of one year. Enrollees would have had to work, volunteer, or participate in other suitable community engagement activities for at least 20 hours per week in order to maintain Medicaid coverage. Exemptions would have been available for various populations, including pregnant women, people with disabilities, and people enrolled in substance abuse treatment.
By 2019, Governor Edwards had backed off from supporting a Medicaid work requirement, and his administration was instead supporting a pilot program to provide job training to some Medicaid expansion enrollees.
Footnotes
- “October 2023 Medicaid & CHIP Enrollment Data Highlights”, Medicaid.gov, Accessed February 2024 ⤶
- “Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment”, KFF.org, Accessed February 2024 ⤶ ⤶
- ”Louisiana Medicaid Renewals Data Reporting“, Louisiana Department of Health, Accessed February 2024 ⤶
- ”Louisiana dental insurance guide 2023” healthinsurance.org, Accessed September 2023 ⤶
- ”Availability of short-term health insurance in Louisiana” healthinsurance.org, April 6, 2023 ⤶

