Medicaid eligibility and enrollment in Maryland
Maryland is automatically enrolling people in QHPs if they lose Medicaid and don’t pick their own new plan


Who is eligible for Medicaid in Maryland?
Maryland’s Medicaid program, which is also called Medical Assistance, has higher income limits than many other states when it comes to Medicaid eligibility for children and people who are pregnant. Individuals with family income up to the following levels are eligible for Medicaid (note that these limits include the build-in 5% income disregard that’s used for MAGI-based Medicaid eligibility):
- 322% of the federal poverty level (FPL) for children ages 0-18
- 264% of FPL for someone who is pregnant (coverage continues for 12 months after the baby is born)
- 138% of FPL for parents and other adults
- Aged, blind, and disabled (ABD) individuals may also qualify for Medicaid; see the income and asset guidelines in the FAQs of the Maryland Department of Health and Mental Hygiene website.
- Maryland helps pay for long-term care for qualifying individuals; see the eligibility criteria and application information.
For ease of reference, the Maryland Health Connection website shows the monthly income limits in terms of dollar amounts rather than percentage of FPL.
for 2026 coverage
0.0%
of Federal Poverty Level
Apply for Medicaid in Maryland
Apply online. Apply in person at a local health department or social services office. Call 1-800-456-8900 and have an application mailed to you. For help applying, call 1-855-642-8572 (1-855-642-8573 for individuals who have hearing difficulty).
Eligibility: Children ages 0-18 with household income up to 317% of FPL. Pregnant women with household income up to 250% of FPL. Adults with household income up to 138% of FPL. Aged, blind, and disabled (ABD) individuals: see income and asset guidelines. See the eligibility criteria for long-term care.
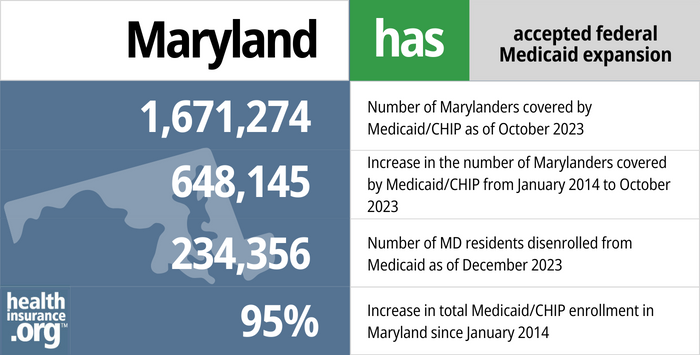
Did Maryland expand Medicaid under the ACA?
Yes, Maryland expanded Medicaid under the ACA. The state’s Medicaid expansion was authorized in May 2013 for a Jan. 1, 2014, start date. Medicaid expansion, which makes Medicaid available to low-income, non-elderly adults, is one of the Affordable Care Act’s main tenets to reduce the nation’s uninsured rate.
- 1,671,274 – Number of Marylanders covered by Medicaid/CHIP as of October 20231
- 648,145 – Increase in the number of Marylanders covered by Medicaid/CHIP from January 2014 to October 20232
- 234,356 – Number of MD residents disenrolled from Medicaid as of December 20233
- 95% – Increase in total Medicaid/CHIP enrollment in Maryland since January 20142
Explore our other comprehensive guides to coverage in Maryland

This guide is designed to help you understand the health coverage options and possible financial assistance available to you and your family in Maryland For many, an Affordable Care Act (ACA) Marketplace (exchange) plan, also known as Obamacare, may be an affordable option.


In 2023, there are four insurers who offer stand-alone individual/family dental coverage through the health insurance Marketplace in Maryland. Our state guide explains the coverage options that may be available to you.


As of early 2023, more than 1.1 million Maryland residents have Medicare coverage.4 Learn more about Medicare in Maryland, including private plan options and Medigap plans.


Maryland residents can buy short-term health plans with durations up to three months.

Frequently asked questions about Maine Medicaid eligibility and enrollment
How do I enroll in Medicaid in Maryland?
In general, you can enroll for Maryland Medicaid online or in person. See below for specifics, which vary for different eligible groups.
- If you are under 65 and don’t have Medicare, apply online through SAIL (Service Access and Information Link) or at www.MarylandHealthConnection.gov.
- Seniors and people who have Medicare can apply for Medicaid using this website.
- Get an application or apply in person at a local health department or social services office. Call 1-800-456-8900 and have an application mailed to you.
- For help applying, call 1-855-642-8572 (1-855-642-8573 for individuals who have hearing difficulty)
- People who are pregnant are encouraged to apply at a local health department. Call 1-800-456-8900 for information
How does Medicaid provide assistance to Medicare beneficiaries in Maryland?
Many people with Medicare receive help through Medicaid with Medicare premium costs, prescription drug expenses, and expenses that Medicare doesn’t cover — such as long-term care.
Our guide to financial resources for Medicare enrollees in Maryland provides an overview of those programs, including Medicare Savings Programs, nursing home benefits, and income guidelines for assistance.
How is Maryland handling Medicaid renewals after the pandemic?
From March 2020 through March 2023, states were prohibited from disenrolling people from Medicaid, even if they no longer met the eligibility requirements. That rule ends March 31, 2023, and states are once again disenrolling people from Medicaid.
Maryland began sending out Medicaid renewal packets in April 2023, and the first round of disenrollments came at the end of May. People who are no longer eligible for Medicaid can transition to a plan offered by an employer if one is available to them. But Maryland Health Connection (the state-run exchange/Marketplace) is automatically enrolling people into private qualified health plans if they’re no longer eligible for Medicaid and don’t pick their own replacement plan. The person has the option of accepting that plan, picking a different plan, or canceling the plan if they have coverage elsewhere. In June 2023, Maryland Health Connection automatically enrolled 3,495 people into QHPs after their Medicaid ended (a total of 8,367 people in Maryland had transitioned from Medicaid to QHPs at that point).
In addition to the automatic enrollment protocol, Maryland Health Connection has an extended special enrollment period for people losing Medicaid during the unwinding of the pandemic-era rules; it continues through July 2024, the same as the special enrollment period that applies in states that use HealthCare.gov. This gives a person additional time to select a new plan if they initially reject the plan that’s automatically selected on their behalf.
Renewals are being spread over a 12-month period, so some Maryland Medicaid (Medical Assistance) enrollees will not receive a renewal packet until late 2023 or early 2024. Until that point, their coverage will continue, even if they no longer meet the eligibility guidelines. But once a member’s renewal is due, they can only continue to receive Medical Assistance coverage if they still meet the eligibility guidelines and also provide the state with requested renewal information (unless the state is able to renew the coverage automatically, in which case the member will be notified that their coverage has been renewed).
Does Maryland Medicaid provide dental benefits for adults?
Yes, as of 2023, Maryland Medicaid includes adult dental benefits. Prior to 2023, since the early 1990s, Maryland had not provided coverage for adult dental care through its Medicaid program (most states provide at least limited or emergency dental coverage for adults enrolled in Medicaid; Maryland was one of just three states that provided no coverage at all). But legislation (HB6 and SB150) was enacted in 2022 to add an adult dental benefit to the state’s Medicaid program as of 2023.
Children with Medicaid already had coverage for dental care in Maryland, as is the case nationwide. And Maryland did implement a program in 2019 to provide dental benefits to Maryland residents age 21-64 who were dually enrolled in Medicaid and Medicare (ie, they are disabled and have low incomes and low assets). But the state estimated that fewer than 39,000 people would be eligible for benefits under that program. Under HB6/SB150, a far larger population of low-income residents gained access to dental care starting in 2023.
Legislation impacting Maine Medicaid
Maryland Medicaid enrollment
Medicaid enrollment in Maryland has grown significantly in the last few years. From late 2013 to early 2023, total enrollment in Maryland’s Medicaid/CHIP doubled. Total Medicaid/CHIP enrollment was 1,706,914 June 2023.
Maryland has used Medicaid managed care since 1991. As of 2022, Medicaid Managed Care Organizations (MCOs) covered about 90% of Maryland’s Medicaid population, while the other 10% were covered under the Medicaid Fee for Service program (the Medicaid FFS program includes elderly enrollees who are also eligible for Medicare, and those who are in long-term care facilities).
There are currently nine health insurance carriers that participate in Maryland’s Medicaid Managed Care program:
- Aetna Better Health
- CareFirst BlueCross Blue Shield Community Health Plan
- Jai Medical Systems
- Kaiser Permanente
- Maryland Physicians Care
- MedStar Family Choice
- Priority Partners
- UnitedHealthcare
- Wellpoint Maryland (formerly Amerigroup Community Care)
Maryland’s leadership and Medicaid expansion
Republican Larry Hogan took over as Maryland’s governor in January 2015, replacing Democrat Martin O’Malley. O’Malley faced a term limit and was not running for re-election; Lt. Gov. Anthony Brown vied with Hogan.
While Hogan frequently criticized O’Malley and Brown over Maryland’s state-run health insurance exchange, Medicaid expansion was not a campaign issue. In fact, Hogan acknowledged that significant changes to Medicaid were unlikely given Democrats’ dominance in the Maryland General Assembly.
Maryland gathered much information about the potential impacts of the ACA’s Medicaid expansion before proceeding with implementation, and the findings were summarized in a Health Affairs blog by an official with the Maryland Department of Health and Mental Hygiene. Maryland estimated that 190,000 Marylanders would gain Medicaid coverage through the expansion by 2020 and took note of a New England Journal of Medicine research showing a 6.1% reduction in mortality for low-income adults covered by expanded Medicaid. Maryland also learned that Medicaid expansion would have a significant positive effect on the state economy, including an estimated $25 billion in federal Medicaid funding and 27,000 new jobs by 2020.
(Medicaid enrollment nationwide is much higher as of 2023 than had been projected, due to the COVID pandemic. So the number of people with Medicaid expansion coverage is higher in nearly every state than officials had projected initially, although that is now declining as states have resumed disenrollments post-pandemic.)
Footnotes
- “October 2023 Medicaid & CHIP Enrollment Data Highlights”, Medicaid.gov, Accessed February 2024 ⤶
- “Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment”, KFF.org, Accessed February 2024 ⤶ ⤶
- ”Medicaid Check-In 2023 – Data“, Maryland.gov, December 2023 ⤶
- “Medicare Monthly Enrollment” CMS.gov, April 2023 ⤶

