Medicaid eligibility and enrollment in South Carolina
South Carolina increased Medicaid eligibility limit for parents of minor children, and extended postpartum coverage to 12 months


Who is eligible for Medicaid in South Carolina?
Although South Carolina still has not accepted federal funding to expand Medicaid eligibility under the ACA, the state did increase the income limits for low-income parents to qualify for coverage. Under the terms of a waiver that was approved by CMS in late 2019, parents and caretakers of minor children are eligible for Medicaid in South Carolina with income as high as 100% of the poverty level.
Here are the current eligibility guidelines for Healthy Connections (South Carolina Medicaid), which include a 5% income disregard (the state also has a resource that shows these limits in terms of monthly income):
- Children with household incomes up to 213% of poverty.
- Parents/caretakers with dependent children, if their household incomes do not exceed 100% of poverty.
- Pregnant women with household incomes up to 199% of poverty. (coverage for the mother continues for 12 months after the baby is born)
Medicaid coverage in South Carolina is not available for non-disabled childless adults, regardless of how low their income is. This is the group most likely to fall into the Medicaid coverage gap, with little in the way of realistic options for health coverage. This problem would be remedied if South Carolina were to accept federal funding to expand Medicaid, but the state has thus far rejected that option.
for 2026 coverage
0.0%
of Federal Poverty Level
Apply for Medicaid in South Carolina
Enroll online at South Carolina Healthy Connections Medicaid or by phone at 1-888-549-0820; or enroll in Medicaid through HealthCare.gov or by phone at 1-800-318-2596
Eligibility: The aged, blind, and disabled. Also children with household incomes up to 208% of FPL; working parents with dependent children with household incomes up to 89% of FPL; jobless parents with dependent children with household incomes up to 50% of FPL; pregnant women with household incomes up to 194% of FPL.
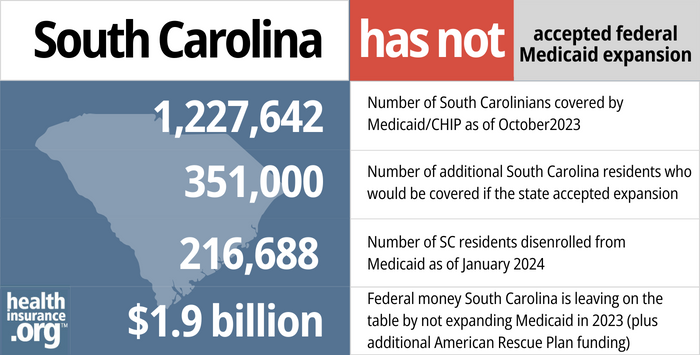
No Medicaid eligibility expansion in South Carolina
South Carolina’s governor and legislature have strongly rejected Medicaid expansion under the Affordable Care Act (ACA). As a result, there are about 105,000 people in the state who are in a “coverage gap.” They are the state’s poorest residents, with incomes under the poverty level, and they have no realistic access to health coverage. They do not qualify for subsidies in the exchange and they also do not qualify for Medicaid. In many cases, they rely on emergency rooms and community health clinics, but future funding for those clinics is in jeopardy too.
Since 2017, Republican Henry McMaster has been the governor of South Carolina (McMaster was the lieutenant governor and took office as the governor when Nikki Haley was appointed by President Trump to be the U.S. Ambassador to the United Nations). McMaster is opposed to Medicaid expansion, as was Haley.
South Carolina’s legislature has not changed its stance on Medicaid expansion. Various bills aimed at expanding Medicaid eligibility had not advanced out of committee as of February 2023 (they include H.3206, S.135, and S.228, along with two bills that call for a statewide advisory referendum about Medicaid expansion on the 2024 ballot: S.59 and H.3070), has not advanced out of committee as of February 2023).
- 1,227,642 – Number of South Carolinians covered by Medicaid/CHIP as of October 20231
- 351,000 – Number of additional South Carolina residents who would be covered if the state accepted expansion2
- 216,688 – Number of SC residents disenrolled from Medicaid as of January 20243
- $1.9 billion – Federal money South Carolina is leaving on the table by not expanding Medicaid in 2023 (plus additional American Rescue Plan funding)4
Explore our other comprehensive guides to coverage in South Carolina

We’ve created this guide to help you understand the South Carolina health insurance options available to you and your family, and to help you select the coverage that will best fit your needs and budget.
Learn about health insurance coverage options in South Carolina.


Looking to improve your smile? Dental insurance may be a smart addition to your health coverage. Our guide explores dental coverage options in South Carolina.


As of September 2022, there were 1,159,851 people enrolled in Medicare in South Carolina.5 Our guide will help you confidently understand Medicare Parts A, B, C and D plans — as well as Medicare supplement (Medigap) plans available in the South Carolina.


South Carolina has its own state regulations regarding short-term health insurance policies. Short-term health insurance in South Carolina can’t last more than 11 months, with a total duration of 33 months (including renewals).6 As of 2023, there were at least five insurers selling short-term health insurance plans in South Carolina.
Learn about short-term insurance regulations in South Carolina.

Frequently asked questions about South Carolina Medicaid
How do I enroll in Medicaid in South Carolina?
Medicaid enrollment is available year-round. South Carolina has taken steps to overhaul its Medicaid enrollment process and is actively working to enroll eligible residents. There are additional employees in the state’s Medicaid call center, an online application process (in addition to HealthCare.gov) and the state is using databases of people who already qualify for other income-based programs like SNAP to help identify residents who are eligible for Medicaid.
- South Carolina Healthy Connections Medicaid has a website where you can enroll online. You can also reach them by phone at 1-888-549-0820.
- You can enroll in Medicaid through HealthCare.gov
- You can enroll over the phone via HealthCare.gov by calling 1-800-318-2596
How does Medicaid provide financial assistance to Medicare beneficiaries in South Carolina?
Many Medicare beneficiaries receive Medicaid’s help with paying for Medicare premiums, affording prescription drug costs, and covering expenses not covered by Medicare – such as long-term care.
Our guide to financial assistance for Medicare enrollees in South Carolina includes overviews of these benefits, including Medicare Savings Programs, long-term care coverage, and eligibility guidelines for assistance.
How is South Carolina handling Medicaid renewals after the pandemic?
Throughout the COVID pandemic, since March 2020, states have been receiving additional federal Medicaid funding, but were also barred from disenrolling anyone from Medicaid prior to April 2023. So even if a person’s circumstances had changed and they were no longer eligible for Medicaid, their coverage was not discontinued. But that continuous coverage requirement ended March 31, 2023, and states could resume disenrollments as early as April 1, 2023.
The federal government has outlined a variety of guidelines that states must follow during the “unwinding” of the continuous coverage requirements. The specifics of South Carolina’s unwinding process can be seen in their state plan document, the SC Healthy Connections Medicaid annual reviews webpage, and a list of frequently asked questions about the unwinding.
Although most states continued to send out renewal packets (but could not disenroll people who didn’t respond or were determined ineligible), South Carolina did not send renewal packets during the pandemic. So that process resumed in South Carolina as of April 2023. The first round of disenrollments won’t come until the end of May, which means that some people will need to have new coverage in place as early as June 1.
According to the state plan document, South Carolina is prioritizing renewals for people they expect to no longer be eligible (for example, a person who has turned 19 or 65 during the pandemic, or who reported a change that would have made them ineligible). But the renewals for the entire Medicaid population will be spread out over the course of the 12-month unwinding period, so some people will not get their renewal notifications until late 2023 or even early 2024. And some people won’t receive a renewal packet, if the state is able to automatically renew their coverage (they will just be notified that their coverage has been renewed).
A person who loses their Healthy Connections coverage during the unwinding period will be able to switch to an employer’s plan, if one is available to them. Those who have become eligible for Medicare during the pandemic will also have a special enrollment period when they can transition to Medicare without a late enrollment penalty. And for those who don’t have access to an employer’s plan or Medicare, coverage is available through HealthCare.gov and most enrollees qualify for substantial financial subsidies. There’s an extended special enrollment period to transition from Medicaid to HealthCare.gov, but it’s important to enroll in the new plan prior to the date that Medicaid terminates, in order to avoid a gap in coverage.
Legislation impacting South Carolina Medicaid
Under Trump admin, CMS approved Medicaid work requirement for low-income parents, but it was not implemented and the Biden administration withdrew approval
The Trump administration approved Medicaid work requirements in several states, although most were either overturned by court rulings or pended by the states, and the rest were suspended amid the COVID pandemic (as noted above, states were not able to disenroll anyone from Medicaid during the pandemic).
In December 2019, when CMS approved South Carolina’s Medicaid work requirement (“community engagement”) proposal, it was the first such approval for a state that hadn’t expanded Medicaid. Because South Carolina hasn’t expanded Medicaid, the state’s Medicaid population consists of low-income people who are children, elderly, disabled, pregnant, or parents of minor children. Adults who don’t fit into one of these categories are not eligible for coverage, no matter how low their income is.
(Medicaid expansion provides coverage for non-elderly adults who don’t fall into the existing eligibility categories (disabled, pregnant, very low-income parents), so the idea behind the work requirements in most states was that since Medicaid expansion applies mostly to non-disabled adults, they should have to work in order to maintain coverage. This logic is flawed in many ways, which have been covered extensively by consumer advocates, but it was the stated premise behind the work requirements that were approved prior to December 2019.)
So if it had been implemented, South Carolina’s Medicaid work requirement would have primarily applied to low-income parents of minor children. Under existing rules, these parents are eligible for Medicaid with income up to the poverty level (about $2,071/month for a family of three in 2023).
But the Biden administration took a different approach, notifying states in early 2021 that work requirements were not aligned with the mission of Medicaid (ie, a health coverage program for low-income people, as opposed to a jobs program). South Carolina soon sent a reply, asking CMS to maintain approval for the work requirement. But in August 2021, CMS notified South Carolina that the work requirement approval was being withdrawn, as was the case in all of the states where work requirements had been approved by the prior administration.
Medicaid eligibility for low-income parents extended to include families with household income up to the poverty level
When South Carolina’s Medicaid work requirement waiver was approved, Medicaid eligibility for low-income parents was set at 67% of the poverty level.
A separate waiver was approved that grants Medicaid eligibility to South Carolina parents with income as high as 100% of the poverty level. Initially, the idea was that parents would have to comply with the state’s new Medicaid work requirement in order to have coverage (see details above). Consumer advocates noted that this could have eventually resulted in as many as 26,000 fewer low-income parents covered under South Carolina’s Medicaid program (the specifics of this were not addressed in the federal approval, as noted here by Georgetown University’s Joan Alker).
But since the Medicaid work requirement was not implemented and approval was eventually revoked by the Biden administration, low-income parents with income up to the poverty level are currently eligible for Medicaid in South Carolina without strings attached.
The second waiver also grants Medicaid eligibility to a “Targeted Adult” population, including those who are chronically homeless, involved with the justice system (as a defendant), or in need of substance use disorder (SUD) treatment. As is the case for low-income parents, these individuals were expected to have to comply with the work requirement unless they qualified for an exemption, but the work requirement was never implemented.
The state estimated that between those two populations (i.e., parents with income that makes them newly-eligible for Medicaid, and the Targeted Adult group), 45,100 people would potentially gain eligibility for Medicaid.
From late 2013 through late 2022, Medicaid enrollment in South Carolina increased by 44%. The income increase for parents to be Medicaid eligibility no doubt played a role in that, but the increase has primarily been driven by the COVID pandemic and the pause on disenrollments from March 2020 through March 2023.
South Carolina Medicaid enrollment
Medicaid enrollment continues year-round, and South Carolina’s poverty rate was 13.8% as of 2019, which is higher than the national average. From the fall of 2013 through late 2022, the population covered by Medicaid in South Carolina grew by nearly 200,000 people — a 44% increase — despite the fact that Medicaid eligibility as called for in the ACA has still not been implemented.
The increase is due largely to the state’s expansion of coverage for low-income parents, as well as the COVID pandemic and the three-year nationwide ban on Medicaid disenrollments during the COVID pandemic.
South Carolina Medicaid history
Medicaid became effective in South Carolina in July 1968, two and a half years after it was available in the first states that implemented it. Eligibility has been improved and expanded over the years through federal mandates that required coverage for children and pregnant women.
A primary provision of the ACA was to expand Medicaid to cover all legally-present residents with incomes up to 138% of poverty, with the federal government paying the full cost of expansion through 2016. After that, the states have gradually taken on a small portion of the cost, but it will never exceed ten percent. It was expected that this landmark expansion of Medicaid would be implemented in every state.
But in 2012, the Supreme Court ruled that states could not be penalized if they chose to not expand their Medicaid programs, and South Carolina is one of the 14 states that has not yet expanded Medicaid.
Former Governor Nikki Haley was staunch in her opposition to Medicaid expansion, although her comments on the issue seemed to indicate that her primary objective was opposing President Obama. In 2013, Haley stated that South Carolina “will not expand Medicaid on President Obama’s watch. We will not expand Medicaid ever.” And Gov. McMaster has maintained that approach. Unfortunately, this means that South Carolina residents are paying federal taxes that are being used to fund Medicaid expansion in other states — and they’re getting nothing for themselves. The state is missing out on $15.8 billion in federal funding over a decade by not expanding Medicaid.
In addition to the financial impact, there’s a human cost to not expanding Medicaid. A White House report in June 2015 noted that expanding Medicaid in South Carolina would save 200 lives per year. Democrats in the state legislature renewed their calls to expand coverage in 2015, but no progress was made during the 2016 legislative session. That has continued to be the case in subsequent sessions, which is unsurprising given the strong Republican majority in the state’s legislature.
Although Medicaid coverage in South Carolina is still limited to a small number of adults in South Carolina, a slight improvement came in December 2014 for Medicaid-eligible adults. Preventive dental care, including cleanings, fillings, and extractions, was added to the existing Medicaid benefits, with up to $750 in annual benefits per member. Previously, this benefit was only provided for children.
Footnotes
- “October 2023 Medicaid & CHIP Enrollment Data Highlights”, Medicaid.gov, Accessed November 2023 ⤶
- ”3.7 Million People Would Gain Health Coverage in 2023 If the Remaining 12 States Were to Expand Medicaid Eligibility“, Matthew Buettgens and Urmi Ramchandani Urban Institute, July 2022 ⤶
- ”Medicaid Annual Eligibility Review Dashboard“, South Carolina Department of Health and Human Services, February 2024 ⤶
- ”Last 11 States Should Expand Medicaid to Maximize Coverage and Protect Against Funding Drop as Continuous Coverage Ends“, Center on Budget and Policy Priorities, January 2023 ⤶
- “Medicare Monthly Enrollment ” CMA.gov, Accessed August 2023 ⤶
- “Availability of short-term health insurance in South Carolina” healthinsurance.org, Jan. 7, 2023 ⤶

