Medicaid eligibility and enrollment in Vermont
Post-pandemic Medicaid disenrollments resume May 31, 2023 in Vermont


Who is eligible for Medicaid in Vermont?
Vermont’s Medicaid program is called Green Mountain Care, and the program for children and pregnant women is called Dr. Dynasaur. In Vermont, income-based Medicaid is available to (these limits include a built-in 5% income disregard that’s used for income-based Medicaid eligibility):
- Adults with incomes up to 138% of federal poverty level (FPL)
- Children with household incomes up to 317% of FPL (premiums suspended during pandemic and and post-pandemic “unwinding” period; will resume in 2024)
- Pregnant women with incomes up to 213% of FPL (coverage for the mother continues for 12 months after the baby is born)
Older adults or individuals who are blind or disabled may also qualify for Medicaid in Vermont. See the Medicaid for the Aged, Blind and Disabled (MABD) page on the Green Mountain Care website for more information.
for 2026 coverage
0.0%
of Federal Poverty Level
Apply for Medicaid in Vermont
Apply for Green Mountain Care and Dr. Dynasaur through Vermont Health Connect.
Eligibility: Adults with incomes up to 138% of FPL; children with household incomes up to 312% of FPL; pregnant women with incomes up to 208% of FPL.
ACA’s Medicaid eligibility expansion in Vermont
Vermont has fully embraced the Affordable Care Act (ACA), including the expansion of Medicaid starting in 2014. But while the state’s uninsured rate is among the lowest in the country, Medicaid/CHIP enrollment was only 19% higher in late 2022 than it had been in late 2013, before Medicaid expansion took effect (nationwide, Medicaid enrollment was up 61% at that point, after increasing sharply during the COVID pandemic).
This is because Vermont had already addressed the issue of health insurance for low-income residents, nearly two decades earlier. So although the state was quick to accept federal funding for Medicaid expansion as called for in the ACA, the uninsured rate among low-income residents was already well below the national average — only 7.2% according to U.S. Census data. By 2014, it had fallen to 5%, and by 2016, it had dropped even lower, to 3.7% — only Massachusetts and Hawaii had lower uninsured rates at that point.
In 1995, the Vermont legislature authorized the creation of Vermont Health Access Plan (VHAP) and Dr. Dynasaur, which is still utilized to provide coverage to children and pregnant women. Dr. Dynasaur provided coverage to children with household incomes up to 300% of poverty, pregnant women with household incomes up to 200% of poverty, and for parents and guardians with incomes up to 185% of poverty.
VHAP provided coverage for other adults with household incomes up to 150% of poverty.
In addition, in 2006, the state created Catamount Health, which allowed residents with incomes up to 300% of poverty to purchase a Catamount plan (provided by either MVP Health or Blue Cross Blue Shield) at a subsidized rate.
As a result of Vermont’s early health care reform, the state’s uninsured rate in 2006 was 10.8% — quite a bit lower than the national average of 15.3% at that point.
Catamount and VHAP were scheduled to end on December 31, 2013, with all the individuals they covered switching to either expanded Medicaid or a subsidized private plan through the exchange. But because of Vermont Health Connect’s rocky rollout, then-Governor Shumlin extended Catamount and VHAP until March 31, 2014 for any residents who were still enrolled in those plans.
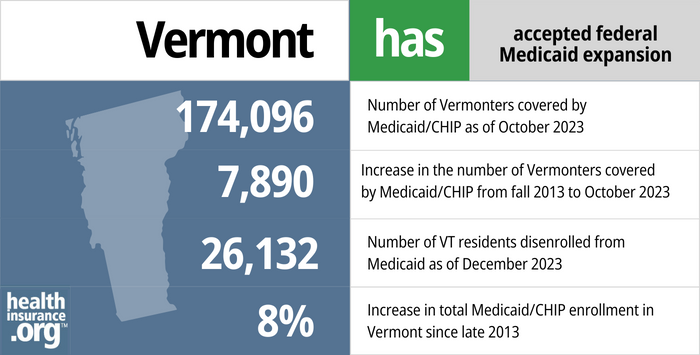
- 174,096 – Number of Vermonters covered by Medicaid/CHIP as of October 20231
- 7,890 – Increase in the number of Vermonters covered by Medicaid/CHIP from fall 2013 to October 20232
- 26,132 – Number of VT residents disenrolled from Medicaid as of December 20233
- 8% – Increase in total Medicaid/CHIP enrollment in Vermont since late 20132
Explore our other comprehensive guides to coverage in Vermont

We’ve created this guide to help you understand the Vermont health insurance options available to you and your family, and to help you select the coverage that will best fit your needs and budget.


In 2023, one insurer offers stand-alone individual/family dental coverage through the health insurance Marketplace, in Vermont.4 Learn about other dental coverage options in the state.


More than 160,000 people in Vermont had Medicare coverage as of early 2023. Most were eligible due to age, but nearly 20,000 were under 65 and eligible for Medicare due to a disability.5Our Vermont Medicare guide explains the various parts of Medicare, coverage options for Medicare Advantage and Part D, and Vermont’s rules regarding Medigap (Medicare Supplement) availability.


No insurers currently offer short-term health insurance in the state. This is due in part to the fact that the state has extensive rules for all health plans, including a requirement that Essential Health Benefits be covered, and a ban on pre-existing condition exclusions.6

Frequently asked questions about Vermont Medicaid
How do I apply for Medicaid in Vermont?
If you’re under 65 and don’t have Medicare, you can apply for Green Mountain Care or Dr. Dynasaur through the state-run exchange, Vermont Health Connect. If you’re 65 or older or have Medicare, use this website to apply for Medicaid.
If you have questions, you can call the Vermont Medicaid office for assistance at 1-800-250-8427.
How does Medicaid provide financial assistance to Medicare beneficiaries in Vermont?
Many Medicare beneficiaries receive Medicaid’s help with paying for Medicare premiums, affording prescription drug costs, and covering expenses not reimbursed by Medicare – such as long-term care.
Our guide to financial assistance for Medicare enrollees in Vermont includes overviews of these benefits, including Medicare Savings Programs, long-term care coverage, and eligibility guidelines for assistance.
How is Vermont handling Medicaid renewals after the pandemic?
Due to the COVID pandemic, Medicaid disenrollments were paused nationwide from March 2020 to March 2023. But states had to resume regular eligibility redeterminations in February, March, or April 2023, and disenrollments could resume as early as April 1, 2023. States than have a one-year “unwinding” period during which they must initiate eligibility redeterminations for everyone enrolled in Medicaid.
Vermont chose to begin the unwinding process in April 2023 (this page has links to numerous FAQs about Vermont’s unwinding process). And their first round of disenrollments will come at the end of May, meaning that some Vermont Medicaid enrollees will need to have other coverage in place by June 2023 in order to avoid a gap in coverage. The state will spread renewals out over a 12-month period, so some enrollees will not get a renewal notice until late 2023 or early 2024, and their coverage will continue until at least their renewal date.
In the initial months of the unwinding period, Vermont is prioritizing renewals for people who reported changes during the pandemic that would make them ineligible for Medicaid (for example, an increase in income) or who aged out of a coverage category (for example, turning 19 or 65). They are also prioritizing renewals for medically needy enrollees with spenddowns (ie, their income is too high for Medicaid eligibility, but they qualify when their medical bills are subtracted from their income).
The state expects to be able to process about 40% of renewals automatically (ex parte), while the other 60% of enrolles will need to provide additional information to the state in order to renew their coverage. People who are no longer eligible will be disenrolled, and so will people who don’t respond to the renewal notification. So it’s essential for enrollees to make sure that their updated contact information, including a cell phone number, is on file with the state Medicaid office.
Tens of thousands of Vermonters (somewhere between 18,000 and 57,000) are expected to be disenrolled during the unwinding process and will need to enroll in other coverage. People who lose their Medicaid or Dr. Dynasaur coverage will be able to transition to an employer’s plan or Medicare (if eligible) or to an individual/family plan obtained via Vermont Health Connect. In each case, however, there’s a limited timeframe during which a person can enroll, so it’s important to sign up for new coverage as soon as the Medicaid termination notice is received (it’s also possible to appeal a Medicaid termination notice, if you believe that you’re still eligible).
Legislation impacting Vermont Medicaid
Medicaid enrollment growth in Vermont
Vermont’s Medicaid enrollment grew by 11% from late 2013 to mid-2016 (and had peaked in early 2016), but enrollment declined after that, likely due to the state’s improved eligibility verification process. As was the case nationwide, Medicaid enrollment grew in Vermont during the COVID pandemic.
All-payer model pilot program underway
Vermont has long been a vanguard when it comes to healthcare reform. And although the state abandoned its push for a single-payer system in late 2014, officials moved forward with their plans for an all-payer model that would merge payments from Medicaid, Medicare, and commercial insurers, paying set rates to all providers in the state via what would essentially be one big accountable care organization.
In September 2016, Vermont received tentative approval from CMS for the waiver that would be needed to coordinate Medicare (which is a federal program) into the all-payer model. In 2017, the state began a pilot program in which 30,000 of Vermont’s 151,000 Medicaid enrollees were covered under the OneCare network of 2,000 providers, with the state paying $93 million to the network for the global care. In 2018, the state tested a program that includes Medicaid, Medicare, and commercially insured patients, with nine of the state’s 14 hospitals participating in the OneCare program, providing care for about 120,000 Vermont residents.
The All-Payer Accountable Care Organization Model Agreement was initially approved from 2018-2022. It has been extended through the end of 2023, and likely through 2024, with plans for a new model to start in 2025.
Medicaid spending drove budget shortfall in the teens; Eligibility redeterminations reduced Vermont Medicaid enrollment
Vermont’s budget was expected to have a $58.5 million shortfall in fiscal year (FY) 2017, which started in July 2016. That was the ninth year in a row that the state’s spending outpaced revenue, and the budget shortfall issue continued into FY 2019. In 2020, there was a hole of nearly $200 million in the year’s state budget, largely due to the COVID-19 pandemic. But the federal coronavirus relief money contributed to a positive budget address from Governor Scott in January 2021.
About $53 million of the projected FY 2017 shortfall was attributed to Medicaid spending, and $36 million of the 2016 fiscal year’s $40 million shortfall was due to Medicaid spending. The federal government paid the full cost of expansion through the end of 2016, but the state had to begin paying 5% of the cost of covering the newly eligible population starting in 2017, and 6% in 2018. In addition, the outreach and enrollment efforts in every state have resulted in people enrolling for the first time in Medicaid despite the fact that they already qualified under the pre-ACA eligibility guidelines. For this population, the states are on the hook for their normal funding split with the federal government.
Former Governor Shumlin proposed a payroll tax in January 2015 (0.7%) to provide additional funding for Medicaid, but lawmakers balked at the idea.
In an effort to rein in spending, Vermont’s Medicaid program began going through eligibility redeterminations for existing enrollees starting in October 2015. Roughly a third of Vermont’s population was on Medicaid, and officials believed that some were not actually eligible for the coverage. As a result of the eligibility redeterminations, the state determined that some young adults had been incorrectly enrolled in Dr. Dynasaur rather than expanded Medicaid (which was fully funded by the federal government through 2016 and 90% funded by the federal government in 2020 and future years) or individual market coverage with subsidies through the exchange.
Eligibility redeterminations played a key role in shrinking total Medicaid/CHIP enrollment back to nearly what it was before Medicaid expansion took effect. Total enrollment was only 1% higher at the end of 2017 than it had been at the end of 2013 (nationwide, it was up 29%). As of December 2022, Vermont’s Medicaid enrollment was up 19% from 2013. That was still far lower than the national average of 61%, but it did represent significant Medicaid enrollment growth during the COVID pandemic.
Vermont Medicaid enrollment numbers
According to Vermont Health Connect enrollment reports, total Medicaid enrollment (adult plus child) through the exchange was 131,993 in December 2014, and had increased to 141,173 by June 2015. Total Medicaid/CHIP enrollment in Vermont stood at 187,174 by August 2015.
Throughout 2014 and 2015, technical problems with Vermont Health Connect, the state’s exchange, made it impossible to accurately verify eligibility when renewing Medicaid coverage. So the state obtained a waiver from the federal government that allowed them to automatically renew Medicaid coverage without verifying eligibility. But by 2016, the state was able to accurately verify eligibility for Medicaid and stopped automatically reenrolling people
By the end of 2017, total Medicaid/CHIP enrollment in Vermont stood at 162,593, following more than a year of eligibility redeterminations to verify that everyone in the program was eligible to remain in it. This was only 1% higher than enrollment had been in late 2013, before Medicaid expansion took effect.
Total Vermont Medicaid enrollment (including CHIP) had grown to more than 192,000 as of late 2022. That was a 19% increase from 2013, due primarily to the COVID pandemic and the resulting pause on eligibility redeterminations nationwide.
Footnotes
- “July 2023 Medicaid & CHIP Enrollment Data Highlights”, Medicaid.gov, Accessed November 2023 ⤶
- “Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment”, KFF.org, Accessed November 2023 ⤶ ⤶
- ”Vermont Unwinding Monthly Report“, Department of Vermont Health Access, October 2023 ⤶
- “Vermont dental insurance guide 2023” healthinsurance.org, Accessed September 2023 ⤶
- “Medicare Monthly Enrollment” CMS.gov, April 2023 ⤶
- “Rule I-2018-03 Short-Term, Limited Duration Health Insurance” Vermont Department of Financial Regulation, Accessed September 2023 ⤶

