Medicaid eligibility and enrollment in Washington
Nearly 552,000 disenrolled from Medicaid by late 2023 due to “unwinding” of pandemic-era rules. Undocumented immigrant adult eligibility begins in mid-2024.


Who is eligible for Medicaid in Washington?
Apple Health (Washington’s Medicaid/CHIP) provides health insurance coverage for qualifying children, pregnant women, parents, seniors, and individuals with disabilities. See the Eligibility page on the Washington State Health Care Authority (HCA) website for details. Below is a summary of income limits for non-elderly adults and children, including an additional 5% income disregard that’s used for eligibility determinations:1
- Adults with incomes up to 138% of the federal poverty level (FPL)
- Children with household incomes up to 215% of poverty
- Pregnant women with incomes up to 198% of poverty. (coverage for the mother continues for 12 months after the baby is born)
- Children are eligible for CHIP with household incomes up to 317% of poverty.
Apple Health is available to children and pregnant women in the allowable income range even if they are undocumented immigrants. And as of July 2024, Apple Health will also be available to undocumented immigrant adults with eligible incomes.1
for 2026 coverage
0.0%
of Federal Poverty Level
Apply for Medicaid in Washington
Apply through HealthCare.gov or by calling 1-800-318-2596 (24 hours a day).
Eligibility: The aged, blind, and disabled. Also, adults with incomes up to 138% of FPL; children with household incomes up to 200% of FPL are eligible for no-premium Medicaid; children with household incomes 200-300% of FPL eligible (with premium); pregnant women with incomes up to 185% of FPL.
ACA’s Medicaid eligibility expansion in Washington
Washington was one of five states that utilized a provision in the ACA that allowed for early expansion of Medicaid, before 2014. From 2011 through 2013, Washington used a waiver from CMS to allow for federal funding to cover adults with incomes up to 138% of poverty who were previously enrolled in three state-run programs (Basic Health, Medical Care Services, or Alcohol and Drug Addiction Treatment and Support Act). And the ACA’s full Medicaid expansion took effect in Washington as soon as it became available, in January 2014.
As a gubernatorial candidate in the fall of 2012, Democrat Jay Inslee expressed his support for Medicaid expansion, and he won the election that November. Soon after Inslee took office, he was encouraging lawmakers to move “quickly” to expand Medicaid in line with the ACA’s provisions. Rather than take a formal vote on the issue however, Medicaid expansion was added as a line item to the state budget (with bipartisan approval), and on June 30, 2013, Washington Governor Jay Inslee approved the budget for the upcoming fiscal year.
Washington has also taken steps to ensure access to Medicaid for children and pregnant women, regardless of immigration status, and that’s being expanded to all adults as of mid-2024.1
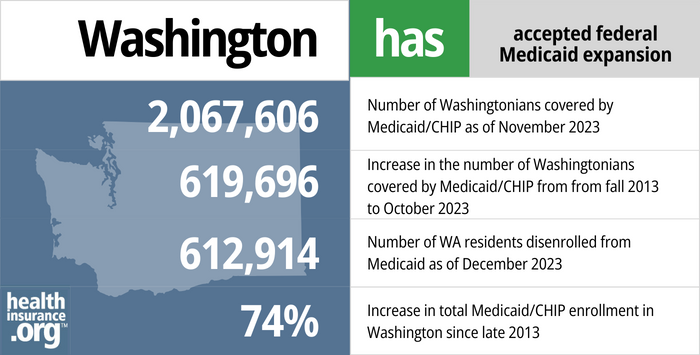
- 2,067,606 – Number of Washingtonians covered by Medicaid/CHIP as of November 20232
- 619,696 – Increase in the number of Washingtonians covered by Medicaid/CHIP from fall 2013 to October 20233
- 612,914 – Number of WA residents disenrolled from Medicaid as of December 20234
- 74% – Increase in total Medicaid/CHIP enrollment in Washington since late 20133
Explore our other comprehensive guides to coverage in Washington

We’ve created this guide to help you understand the Washington health insurance options available to you and your family, and to help you select the coverage that will best fit your needs and budget.
Learn about health insurance coverage options in Washington.


In 2023, four insurers offer stand-alone individual/family dental coverage through Washington Health Plan Finder.5 Our guide will help you understand your dental coverage options in Washington.


Nearly 1.5 million Washington residents were enrolled in Medicare as of 2023.6 Our Washington Medicare guide explains the various parts of Medicare, coverage options under Medicare Advantage and Part D, and New Jersey rules regarding Medigap (Medicare Supplement) availability.


Washington implemented fairly strict new rules for short-term health insurance in 2021. And by mid-2022 there were no longer any insurers offering short-term health insurance in the state.7

Frequently asked questions about Washington Medicaid
How do I apply for Medicaid in Washington?
In Washington State, most Medicaid enrollment is managed through the state-run exchange, Washington Healthplanfinder. Unlike private health plans, Medicaid enrollment continues year-round; there is no specific time during the year that you must enroll.
But if you’re 65 or older or have Medicare, use this website to apply for Medicaid and several other social services benefits. You can also request an application by calling 1-877-501-2233. Visit a Department of Social and Health Services (DSHS) Community Services Office to apply in-person for Medicaid for the aged, blind, and disabled; visit a Home and Community Services Office to apply for long-term care benefits.
How does Medicaid provide financial assistance to Medicare beneficiaries in Washington?
Many Medicare beneficiaries receive Medicaid financial assistance that can help them with Medicare premiums, lower prescription drug costs, and pay for expenses not covered by Medicare – including long-term care.
Our guide to financial assistance for Medicare enrollees in Washington includes overviews of these programs, including Medicaid long-term care benefits, Extra Help, and eligibility guidelines for assistance.
How is Washington handling Medicaid renewals after the pandemic?
During the COVID public health emergency, states did not disenroll anyone from Medicaid, even if they no longer met the eligibility criteria. That continuous coverage rule was in place for three years, from March 2020 through March 2023. But in the spring of 2023, states began disenrolling people who were no longer eligible for Medicaid.
Washington began redetermining eligibility in May 2023, and the first disenrollments were effective as of June.3 By November 2023, nearly 552,000 people had been disenrolled from Apple Health, the majority of whom did not complete their renewal packets4 (and thus may or may not actually still be eligible for coverage).
States have a year to initiate eligibility redeterminations for everyone enrolled in Medicaid, in a process that’s being referred to as “unwinding” the pandemic-era continuous coverage rule. So some people will not get a renewal notice until early 2024, and their coverage will remain in effect until if and when they either don’t respond to an eligibility redetermination notice or respond and are found to no longer be eligible.
People who are no longer eligible for Apple Health can secure new coverage, either through an employer, Medicare, or Washington Healthplanfinder (the state-run exchange/Marketplace). A person’s circumstances will determine which of those coverage options is available to them, but all of them offer a special enrollment period during which a person will be able to transition to the new coverage after losing Apple Health coverage.
People who are eligible for Cascade Care savings can enroll in that coverage at any time (Cascade Care savings is available through Washington Healthplanfinder for people who earn up to 250% of the poverty level and who select a standardized silver or gold plan). People enrolling through Washington Healthplanfinder who aren’t eligible for Cascade Care savings will be eligible for a special enrollment period due to the loss of their Apple Health coverage. Employer-sponsored health plans must have at least a 60-day special enrollment period for people who lose Medicaid. And Medicare is offering a six-month enrollment period for people who are losing Medicaid and are now eligible for Medicare.
If a person loses Apple Health but is still eligible (perhaps because they didn’t respond to the renewal packet in time), they have 90 days to complete the renewal and their coverage will be reinstated as if it never ended.
Legislation impacting Washington Medicaid
More than 2 million enrolled in Apple Health as of late 2023
By late 2023, total enrollment in Apple Health stood at more than 2 million people.3 Enrollment had been higher in early 2023, but enrollment had begun to decline by the fall of 2023, due to post-pandemic eligibility redeterminations and disenrollments.4
Even with the disenrollment process underway, Apple Health enrollment was 75% higher in the fall of 2023 than it had been in the fall of 2013.6
Footnotes
- Noncitizens. Washington State Health Care Authority. Accessed January 2024 ⤶ ⤶
- Apple Health Client Eligibility Dashboard. Washington State Health Care Authority. Accessed January 2024. ⤶
- Total Monthly Medicaid & CHIP Enrollment and Pre-ACA Enrollment, KFF.org, Accessed January 2024. ⤶ ⤶
- Apple Health Data During the Unwind. Washington State Health Care Authority. Accessed January 2024 ⤶
- “Washington dental insurance guide 2023” healthinsurance.org, Accessed September 2023 ⤶
- “Medicare Monthly Enrollment” CMS.gov, April 2023 ⤶
- “Availability of short-term health insurance in Washington” healthinsurance.org, Sept. 5, 2023 ⤶

