Key takeaways
- Both you and the IRS will get a tax form showing whether you had health coverage during the previous year.
- Health insurance exchanges track enrollees and report the information to the IRS.
- There is no longer a penalty for being uninsured in most states, but the IRS will continue to receive enrollment and coverage offer reports from exchanges and employers.
Q. Who is keeping track of whether I buy health insurance through the exchanges?
A. Regardless of where you get your health insurance, you (and the IRS) will receive a tax form from your employer, insurance company, or exchange each year showing that you had coverage during the previous year. The information on these forms is used to complete your tax return and – if applicable – reconcile your premium subsidy on your return.
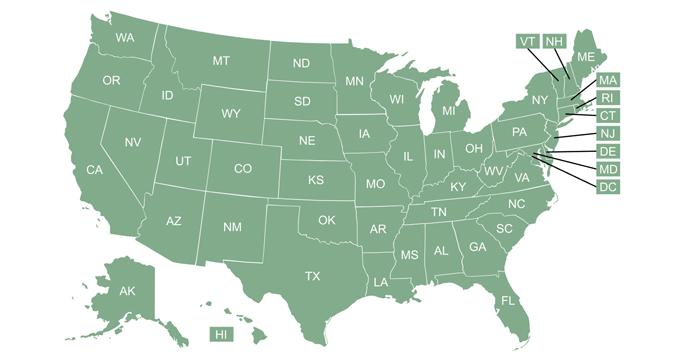
The health insurance exchanges keep track of who gets exchange-based coverage, and report that information to the IRS. But health insurers and employers also report information to the IRS, for people who get their coverage elsewhere. This information is used by the IRS to ensure that large employers are complying with the employer mandate, and that premium subsidies in the exchange aren’t provided to people who have access to employer-sponsored coverage.
Starting with 2019 tax returns (filed in early 2020), tax filers no longer face a federal penalty if they were uninsured during the year, but Forms 1095-A, B, and C are still distributed to exchange enrollees, health plan members, and employees. And Form 8962 is still used to reconcile premium subsidies that are provided via the exchanges.
(For 2020 coverage, people who would normally have to repay some or all of their advance premium tax credits to the IRS did not have to do so. Those individuals simply didn’t have to file Form 8962 at all. People who were eligible to claim additional premium tax credit amounts for 2020 were able to use Form 8962 to do that, as is always the case.)
For 2020 coverage, Form 1095-B had to be provided to health plan members and the IRS by March 2, 2021; Form 1095-C had to be provided to employees and the IRS by March 2, 2021; Form 1095-A had to be provided to exchange enrollees and the IRS by February 1, 2021 (this form is used to complete Form 8962; as noted above, the only tax filers who needed to submit Form 8962 for 2020 coverage are those who were eligible to claim additional premium tax credits from the IRS during the tax filing season, because the amount that was paid on their behalf via the exchange in 2020 was too small).
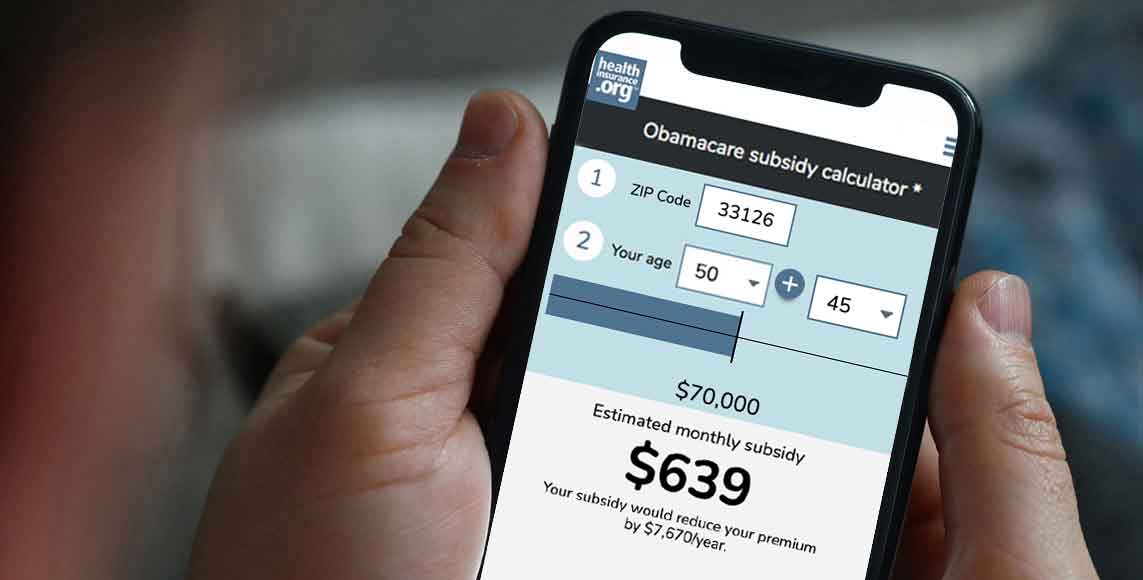
Although there is no longer a penalty (in most states) for being uninsured, health insurance reporting to the IRS is mostly unchanged. Employers still have to report coverage offers to the IRS and employees, as subsidy eligibility is based in part on whether the person has access to an employer-sponsored plan. And exchanges still have to provide the information that individuals and the IRS need in order to reconcile subsidy amounts.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.