Please provide your zip code to see plans in your area.
Call our agency partners
866-553-3223
Featured

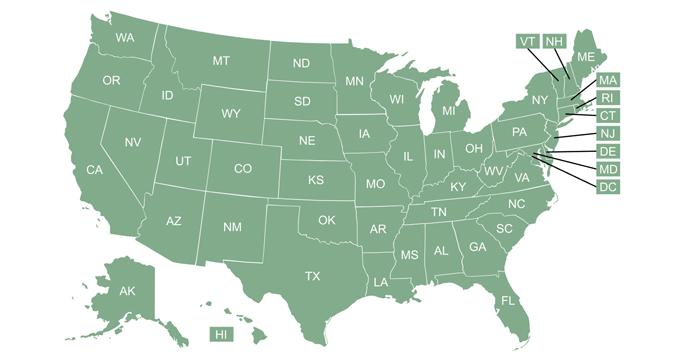
What are the deadlines for the ACA’s open enrollment period?
A list of the open enrollment deadlines for enrollment in 2023 ACA-compliant health insurance in every state. Open enrollment ended on January 15, 2023 in most states.
Featured

Applying for ACA Coverage?
Understanding how small differences in projected income can have a large impact on your health plan costs can be key to obtaining affordable coverage.
A trusted independent health insurance guide since 1994.
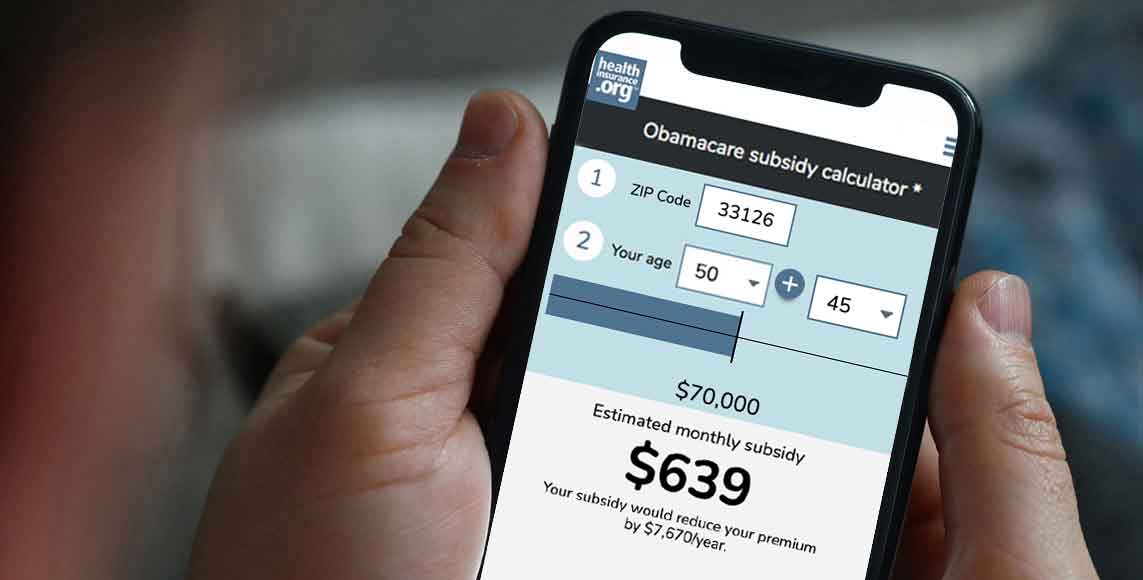
Ready to enroll? See how much you could save on 2023 coverage.
health reimbursement arrangement (HRA)
What is a health reimbursement arrangement (HRA)?
An HRA (health reimbursement arrangement) is a pre-tax way for employers to reimburse employees for qualified medical expenses incurred by the employee or their spouse or dependents. The rules for HRAs are outlined in IRS Publication 969. HRAs are sometimes referred to as health reimbursement accounts.
- HRAs must be funded entirely by the employer, so nothing is deducted from the employee’s paycheck.
- The HRA contribution that the employer makes is not counted in the employee’s income.
- Unlike FSAs and HSAs, there’s no upper limit on how much employers can contribute to their employees’ HRAs, although non-discrimination rules apply. There are also no minimum contribution requirements for HRAs.
- Although the IRS defines what constitutes qualified medical expenses, employers can further limit the expenses for which employees can seek reimbursement under their HRA.
- In June 2020, the IRS proposed regulations that would allow employers to use HRAs to reimburse employees for direct primary care fees and health care sharing ministry fees.
- In order to be reimbursed, an employee has to provide documentation showing that they incurred an eligible expense.
- In most cases, an HRA benefit makes an employee ineligible to contribute to an HSA (even if they have an HSA-compliant high-deductible health plan), although there are some limited types of HRAs that can be used in conjunction with an HSA.
- Under federal rules related to the implementation of the ACA, employers were not allowed to offer an HRA unless it was integrated with an employer-sponsored group health insurance plan. These rules were relaxed in 2017 for small employers (see QSEHRA) and further relaxed, for all employers, as of 2020 (see ICHRA).
- As of 2011, the ACA prohibited the purchase of over-the-counter medications with HRA funds, unless a doctor wrote a prescription for them. But Section 4402 of the 2020 Coronavirus Aid, Relief, and Economic Security (CARES) Act changed that. The CARES Act, signed into law in March 2020 to address the COVID-19 pandemic, eliminated subsection (f) of Section 106 of the Internal Revenue Code. That section had previously prohibited the purchase of non-prescription over-the-counter medications with HRA money (pre-CARES Act, it specified that “reimbursement for expenses incurred for a medicine or a drug shall be treated as a reimbursement for medical expenses only if such medicine or drug is a prescribed drug (determined without regard to whether such drug is available without a prescription) or is insulin.”)
- Section 4402 of the CARES Act also changed the rules to allow menstrual products to be purchased with FSA funds. The new rules allowing HRA enrollees to submit receipts and be reimbursed by their HRAs for over-the-counter medications and menstrual products are retroactive to January 1, 2020. And these are permanent rule changes (ie, they will remain in place even after the COVID-19 emergency period ends).
Related articles
This SEP means you won't have to wait until the next open enrollment if you're offered reimbursement for health premiums through a QSEHRA or ICHRA.
Outside of ACA's annual open enrollment, you can still enroll or change plans if you experience a qualifying event.
Sweeping health reform legislation delivered a long list of provisions focused on health insurance affordability, consumer protections.
Why do small-business owners go to the trouble of setting up small-group coverage?