Please provide your zip code to see plans in your area.
Featured

Featured


Medicaid coverage in New Hampshire is no longer being automatically renewed like it was during the COVID-19 pandemic. Things are returning to normal beginning in 2023.
Learn how the end of continuous Medicaid coverage in New Hampshire may impact you and your family.
We can help you stay covered.
The end of continuous Medicaid coverage in New Hampshire
Home > medicaid-redetermination > Medicaid Redetermination – New Hampshire
Why is New Hampshire continuous Medicaid
coverage ending in 2023?
If you have Medicaid in New Hampshire, you may have received a yellow notice that says “continuous Medicaid coverage is ending.”
Since 2020, because of the pandemic, people could keep their Medicaid coverage without going through the normal redetermination process to verify eligibility. The continuous Medicaid coverage requirement helped millions of people continue to access the healthcare they needed during the pandemic.
Now, that requirement is ending, and state Medicaid departments nationwide — including the New Hampshire Department of Health and Human Services (DHHS) — are sending out requests for redeterminations to see if people still qualify for Medicaid.
Get coverage through your employer
You may be able to get health insurance through an employer, or the employer plan of your spouse or parent. There is a special enrollment window for employer-sponsored coverage. But don’t wait to act – that window only lasts for 60 days for people who have lost Medicaid coverage.
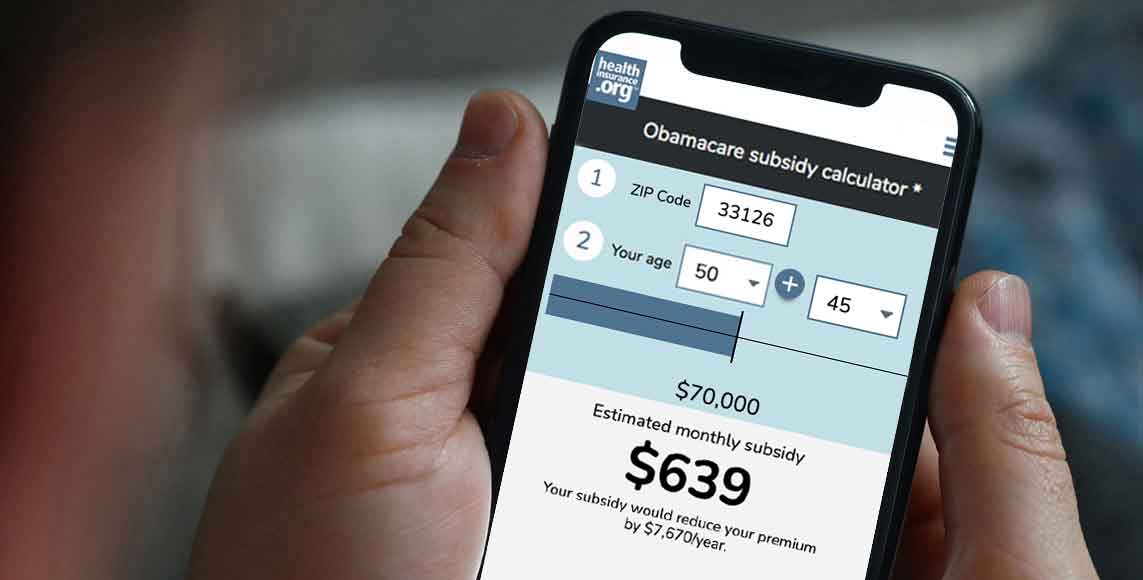
A New Hampshire marketplace plan
Find a plan for 2023 on the New Hampshire health insurance marketplace. Marketplace plans include essential benefits required by the Affordable Care Act (ACA). You qualify for a special enrollment period for these plans when you lose Medicaid coverage. You may even qualify for financial assistance to help cover the cost of marketplace coverage.
See if you qualify for financial help
Are you eligible for Medicare?

Determining if you’re still eligible for Medicaid coverage in New Hampshire
If you are mailed a yellow notice from the New Hampshire Department of Health and Human Services (DHHS), respond right away. You can complete your redetermination by mail or online through the NH Easy Gateway to Services. If you don’t already have an NH Easy account, you can create one online at https://nheasy.nh.gov. Once you have an account, you can upload verifications and other information you have been asked to provide.
Resources:
- Send requested verifications: Centralized Scanning Unit, PO Box 181, Concord, NH 03302.
- Find a local office: Visit the DHHS website.
- For additional help: DHHS Customer Service Center (1-844-275-3447)
How to complete a redetermination to keep your Medicaid coverage in New Hampshire
Keep an eye on your mailbox
New Hampshire announced on Jan. 31, 2023, that it would be mailing letters in the next several months. The continuous coverage requirement in New Hampshire ends March 31, 2023. The state then resumes regular Medicaid eligibility operations on April 1, 2023.
Sign up for a NH Easy account
The NH Easy Gateway to Services is New Hampshire’s electronic application system. The NH Easy site also allows you to check your eligibility and track your application status. You can also use the online system to apply for programs including the Supplemental Nutrition Assistance Program (SNAP), child care assistance, and Medicaid.
Provide requested verifications
DHHS may want more information about your income and resources, and residency – the main criteria New Hampshire uses to determine Medicaid eligibility. Respond right away to any requests for information, whether they come in the mail or to your NH Easy account.

Appeal the decision, if necessary
You can appeal the decision to end your Medicaid coverage if you believe you still qualify for coverage. You need to file the appeal within 30 days of the date printed on the notice of decision you get.
(NOTE: The unwinding of continuous Medicaid coverage does not impact the Supplemental Nutrition Assistance Program (SNAP), although the additional pandemic-related SNAP benefits ended in February. And the scheduled end of the federal public health emergency on May 11, 2023, will affect SNAP eligibility for some people. Watch for letters and notices from your state to stay up-to-date on what you need to know about SNAP.)
When might I lose Medicaid coverage?
If you live in New Hampshire, you could lose Medicaid coverage as early as April 1, 2023. New Hampshire is one of the first states to resume regular disenrollments, effective April 1. But eligibility redeterminations for the state’s Medicaid population will be spread out over a 12-month period. That means some enrollees who are no longer eligible will not actually lose their Medicaid coverage until late 2023 or early 2024.
Helpful links
Jump to
- Why is New Hampshire continuous Medicaid coverage ending in 2023?
- Options if you no longer qualify for Medicaid
- Determining if you’re still eligible for Medicaid coverage in New Hampshire
- How to complete a redetermination to keep your Medicaid coverage in New Hampshire
- When might I lose Medicaid coverage?