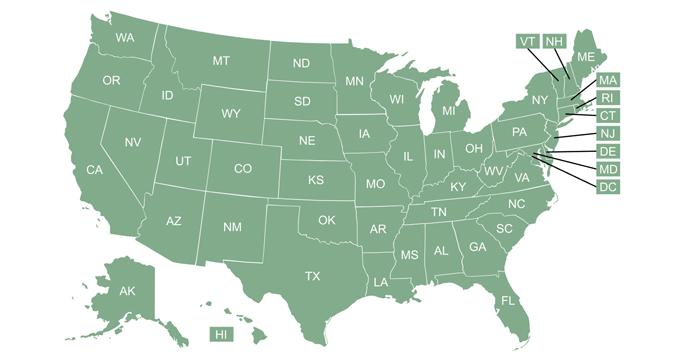
Q. What type of health insurance exchange/marketplace does my state have?
A. For the 2023 plan year, there are 18 fully state-run health insurance marketplaces (SBMs), three state-based marketplaces that use the federal platform (SBM-FP), six state-federal partnership marketplaces, and 24 fully federally-run marketplaces (FFMs). (The federal platform is HealthCare.gov; note that “Exchange” and “Marketplace” mean the same thing, so you’ll also see people use the acronyms SBE, SBE-FP, and FFE)
Three of the states that now have SBMs (Kentucky, Maine, and New Mexico) had SBM-FPs as of 2021, but created their own state-run exchange platforms that were up and running as of the fall of 2021. Virginia plans to join them in the fall of 2023.
And in the rulemaking process for 2024 coverage, HHS has proposed a more lenient approval process timeline for states that are transitioning away from the federally-run exchange in order to establish their own exchange and/or exchange platform. The current rules require a state to have federal approval or conditional approval at least 14 months before the start of open enrollment if they’re transitioning from an SBM-FP to an SBM, and at least three months before the start of open enrollment if they’re transitioning from the FFM to an SBM-FP. But HHS has proposed that the approval or conditional approval would simply have to be received before the start of open enrollment. States would continue to go through the same intensive process of working with HHS to ensure a smooth transition and well-functioning exchange, but would not have to obtain approval more than a year in advance in order to establish an SBM.
This page describes each state’s exchange management approach as of the 2023 plan year. We’ve also included, below, a summary of how this has changed over time, as several states have transitioned to or from HealthCare.gov over the years.
There was initially a trend of states abandoning their own enrollment platforms and opting for HealthCare.gov instead. But we’re seeing the opposite happening in the 2020s, with a growing number of states choosing to leave HealthCare.gov and operate their own exchanges with their own enrollment platforms. This gives a state added flexibility (for example, the opportunity to extend open enrollment) and control, and states are also finding that it’s less costly to operate their own exchanges. And as noted above, HHS has proposed a relaxed approval timeline for this process in future years.
How does a state's exchange model affect the open enrollment schedule?
States that use the federally-run marketplace – including SBM-FPs and partnership marketplaces – have to follow the open enrollment schedule set by HHS. For coverage effective in 2022 and future years, the enrollment schedule in these states is November 1 through January 15.
States that run their own exchange platforms can set their own open enrollment schedules, as long as the final deadline isn’t earlier than December 15. But most of them have opted for an enrollment window that’s at least as long as the enrollment window being used by HealthCare.gov. For 2022 and 2023 coverage, Idaho was the only state-run exchange that chose to have an earlier deadline.
Here’s how each state’s exchange is run, as of the 2023 plan year:
SBMs: State-run marketplaces (these states have their own enrollment websites)
- California
- Colorado
- Connecticut
- District of Columbia
- Idaho
- Kentucky
- Maine
- Maryland
- Massachusetts
- Minnesota
- Nevada
- New Jersey
- New Mexico
- New York
- Pennsylvania
- Rhode Island
- Vermont
- Washington
SBM-FPs: State-based marketplaces that use the federal enrollment platform (HealthCare.gov)
- Arkansas
- Oregon
- Virginia* (legislation has been enacted to create a state-run exchange that will be active by the fall of 2023)
Partnership exchanges (these states use the federal HealthCare.gov enrollment platform)
Federally-run marketplace (these states rely entirely on HealthCare.gov)
- Alabama
- Alaska
- Arizona
- Florida
- Georgia
- Hawaii
- Indiana
- Kansas*
- Louisiana
- Mississippi
- Missouri
- Montana*
- Nebraska*
- North Carolina
- North Dakota
- Ohio*
- Oklahoma
- South Carolina
- South Dakota*
- Tennessee
- Texas
- Utah
- Wisconsin
- Wyoming
(States with an asterisk have a marketplace plan management exchange. Their exchanges are federally-run, but the state retains oversight of the plans, and is active in certifying QHPs for sale in the exchange.)
How has management of the marketplaces changed over time?
The exchanges/marketplaces debuted in the fall of 2013, providing coverage for the 2014 plan year. Since then, several states have made changes to their marketplace management. Some have opted to move away from HealthCare.gov and operate their own exchange, while others have taken the opposite course, abandoning a state-run enrollment platform in favor of using HealthCare.gov.
For the 2015 plan year:
- Idaho used HealthCare.gov for enrollment in 2014, but switched to being a fully state-run exchange prior to the 2015 open enrollment period.
- Nevada and Oregon both had state-run exchanges in 2014, but due to technical difficulties, they both opted to become federally-supported state-based exchanges (SBM-FPs) prior to the 2015 open enrollment period (Nevada has since switched back to having a fully state-run exchange).
For the 2016 plan year:
- Hawaii opted to transition to an SBM-FP, abandoning its state-run enrollment platform (as noted below, Hawaii dropped the state-run aspect altogether the following year).
For the 2017 plan year:
- Arkansas switched from having a state-federal partnership exchange to an SBM-FP (enrollment continued to be via HealthCare.gov, so there was no change from a consumer perspective).
- Hawaii switched from an SBM-FP to the federally-run exchange (enrollment continued to be via HealthCare.gov, so there was no change from a consumer perspective).
- Kentucky switched from a state-based exchange to an SBM-FP (Kentucky is planning to revive its fully state-run exchange and Kynect enrollment platform in time for the 2022 plan year).
For the 2020 plan year:
Exchange management stayed unchanged for a few years. But several changes took effect in the fall of 2019, for the 2020 plan year:
- Nevada switched to a fully state-run exchange, after having an SBM-FP since 2015. Nevada enrollees now use Nevada Health Link instead of HealthCare.gov.
- New Jersey transitioned to an SBM-FP, after having a federally-run marketplace since 2014 (federal approval for this was granted in October 2019; enrollees continued using HealthCare.gov, but as described below, the state will no longer use HealthCare.gov as of the 2021 plan year).
- Pennsylvania also transitioned to an SBM-FP, after having a fully federally-run marketplace in previous years. And just like New Jersey, Pennsylvania will stop using HealthCare.gov in the fall of 2020.
For the 2021 plan year:
The following changes occurred in the fall of 2020:
- Pennsylvania transitioned to a fully state-run exchange, called Pennie (residents no longer use HealthCare.gov).
- New Jersey transitioned to a fully state-run exchange, utilizing the GetCoveredNJ platform (residents no longer use HealthCare.gov).
- Virginia transitioned to an SBE-FP (residents continue to use HealthCare.gov for enrollment at this point, but Virginia plans to transition to a fully state-run exchange with its own enrollment platform by the 2023 plan year).
- Maine transitioned to an SBM-FP, and plans to have a fully state-run exchange by the fall of 2021. Legislation was enacted in Maine in 2020 to move forward with the process of creating a state-run exchange. Maine did not receive federal Navigator funding in August 2020, because the state was going to be operating its own state-run exchange (albeit with the HealthCare.gov platform used for enrollment) by the time open enrollment began in November 2020, meaning that Maine became responsible for its own Navigator program funding.
For the 2022 plan year:
New Mexico, Maine, and Kentucky transitioned away from HealthCare.gov as of November 1, 2021, for people enrolling in coverage with a 2022 effective date. All three states used the SBM-FPs for the 2021 plan year.
Anticipated changes for future years:
Virginia plans to have a fully state-run exchange by the 2024 plan year.
Oregon, which has an SBM-FP, is also considering a future switch to its own enrollment platform.
Change to SHOP (small business) exchange management
Arkansas, Mississippi, and Utah were all running their own SHOP exchange (the platform for small businesses to enroll in coverage), but switched to using the federal platform or a direct-to-carrier process by 2018. But by that point, even the federal platform for small business enrollment was no longer functioning as it had in past years, and small group enrollment had switched to a direct-to-carrier process in nearly every state.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org. Her state health insurance marketplace updates are regularly cited by media who cover health reform and by other health insurance experts.