11 steps toward getting your financial house in order
- Check which providers are in your health plan’s network.
- Know your plan’s out-of-pocket costs before you need care.
- If your income changes, notify your exchange.
- Improve your ACA coverage by switching plans (if you’re eligible).
- If you can’t afford an ACA plan, consider short-term health insurance.
- Consider pairing a health savings account with a high-deductible health plan.
- If you have qualified health expenses, consider using funds from your HSA.
- If you have an account, review your HSA contribution level.
- Remember that HSA funds roll over each year and continue to grow.
- Evaluate – or reevaluate – your need for life insurance.
- Consider disability insurance.
Even before 2023 arrives, millions of Americans have made a resolution: to establish a solid financial footing for the year ahead by selecting reliable individual health insurance coverage during open enrollment — a particularly important decision as the global pandemic drags on. But while choosing the right health plan for your needs is a step in the right direction, it’s only one move of many you can take toward getting your financial house in order.
So how can you build on that first buying decision? A quick insurance tune-up – one that incorporates not only health insurance, but tools such as health savings accounts, life insurance, and disability insurance – can save you from headaches in the months ahead.
Be particular about health insurance
Open enrollment for 2023 health insurance continues until January 15, 2023 in most states, although you’ll likely need to enroll or switch plans by December 15 to have your new plan take effect January 1.
Premium subsidies continue to be larger and more widely available, thanks to the American Rescue Plan and the Inflation Reduction Act. And there have been some changes in terms of the insurers offering plans in the marketplaces in many areas for 2023, including some insurer exits and some new participants (which can affect subsidy amounts in some cases). Now is a great time to review your health insurance, make sure you understand the details, and switch to a different plan if it will better meet your needs.
1. Know your plan’s network.
You should definitely know where the nearest in-network hospital is, and which urgent care facilities are in your health plan’s network. You’ll also want to make sure your preferred primary care and specialists are in-network with any health plan you’re considering for 2023.
If you choose to use out-of-network medical providers, you can expect to receive a balance bill, on top of the normal cost-sharing you’d have to pay when using an in-network provider.
But fortunately, federal rules took effect in 2022 to prevent “surprise balance billing.” That means patients are no longer subject to out-of-network balance bills in emergency situations, or in situations where they go to an in-network hospital but unknowingly receive care from an out-of-network provider while they’re there.
2. Understand your plan’s out-of-pocket costs.
Do you know how much you’ll need to pay if you end up needing various medical services? Unexpected bills are never fun, so it’s good to know the basics in advance.
Make sure you understand your plan’s deductible and copays – and to which services they each apply – as well as the coinsurance percentage and the maximum out-of-pocket amount (keeping in mind that the cap on your out-of-pocket costs only applies to covered, in-network services).
Be aware that these amounts might be changing for the coming year, even if you’re renewing your existing plan (health plans can modify their benefits from one year to the next). As always, it’s worth shopping around to see if there are better options available. This is especially true for 2023, given the influx of new insurers into the marketplaces in many areas, along with some big-name insurer exits (if your insurer exits the exchange and you don’t pick your own replacement plan, the exchange will pick one for you — but it may not be the option that will best fit your needs).
3. Stay on top of your premium subsidy.
Obamacare subsidy calculator *
You’ll eventually have to reconcile your subsidy amount with the IRS, but notifying the exchange in real-time when you have a change in income will make for fewer surprises next year at tax time.
4. Switch plans if necessary.
For most Americans shopping in the individual market, the opportunity to switch plans occurs in the fall, during open enrollment. (That’s November 1 through January 15 in most states, if you’re buying your own health insurance.).
But if you experience a qualifying event outside of that window, you’ll have an opportunity to switch plans at that point. (You may be limited to switching to a plan at the same metal level you already have, depending on the nature of the qualifying event).
If you think you might like to switch plans, our guide to open enrollment will answer a lot of the questions you might have about the logistics and how you should go about determining which plan will best fit your needs.
5. Stay covered – even if it’s temporary coverage.
An estimated 8.3% of Americans didn’t have health insurance at any point during 2021. Some have chosen to go without coverage, while others have been priced out of the market. The good news is that the American Rescue Plan has made self-purchased health coverage much more affordable than it used to be, particularly for people whose income was previously just a little too high to qualify for subsidies.
 So if you haven’t shopped for health insurance lately, you’ll want to check again to see your options for 2023. You might be pleasantly surprised to see how affordable it is, with the larger and more widely available subsidies in place.
So if you haven’t shopped for health insurance lately, you’ll want to check again to see your options for 2023. You might be pleasantly surprised to see how affordable it is, with the larger and more widely available subsidies in place.
However, if you’re ineligible for subsidies but in fairly good health, obtaining coverage under a short-term health insurance plan is far better than remaining uninsured. Short-term plans don’t cover some of the ACA’s essential health benefits, and they generally don’t cover pre-existing conditions — but when it comes to getting your financial house in order, some safety net is better than none.
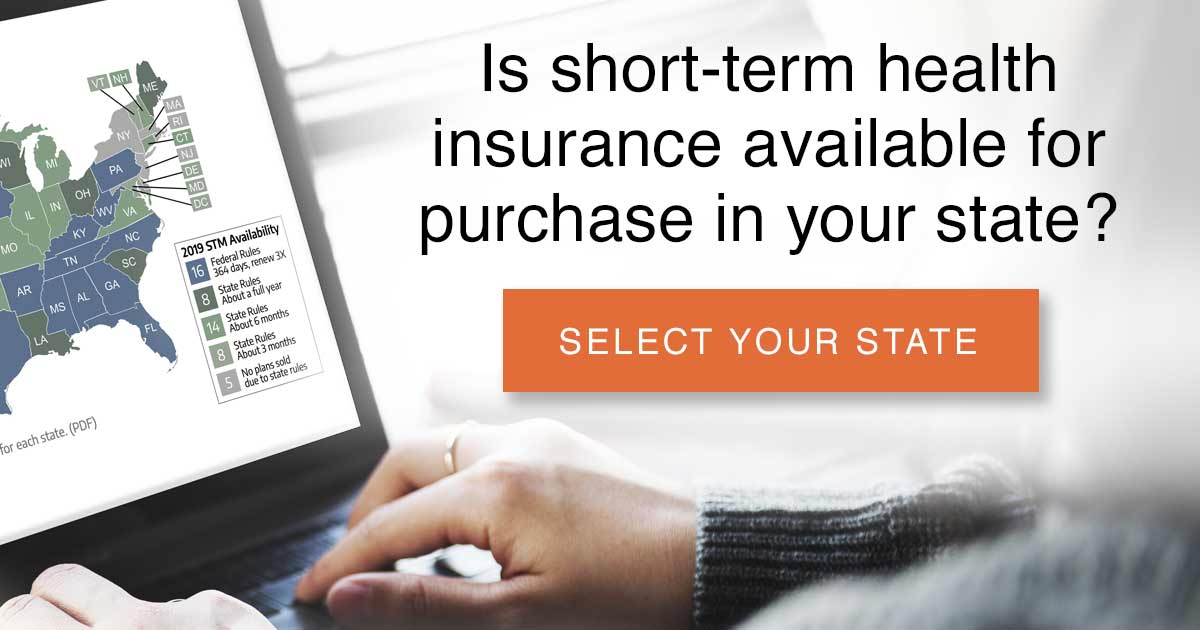
And unlike ACA-compliant plans that can only be purchased during open enrollment — or a special enrollment period, if you experience a qualifying event — short-term plans can be purchased year-round. These plans are available in most states, with initial terms that can be up to a year if your state allows it (click on your state on this map to see the availability of short-term plans and how they’re regulated).
Tap into the power of HSAs
6. Pair your HDHP with a health savings account.
If you have an HSA-qualified health insurance plan (a high-deductible health plan or HDHP), you should – if you haven’t already – consider pairing it with a health savings account (HSA). A high-deductible plan is a term specifically defined by the IRS – it doesn’t mean just any plan with a high deductible, so check with your insurer if you’re in doubt.
An HSA is an excellent financial tool for saving pre-tax money to cover upcoming medical costs (including those you might incur in the distant future), and it can also serve as a backup retirement account.
7. If you have an HSA, stash some money in it.
If you have access to an HSA you can’t afford not to fund it. Sooner or later, you’re going to have out-of-pocket medical expenses. Being able to pay them with pre-tax dollars will be easier on your wallet, and having the money on hand will be a stress-reliever when you need it most.
But remember: if you withdraw HSA funds and don’t use them to pay for qualified medical expenses, you’ll pay income tax and a penalty. (If you’re 65 or older, the penalty no longer applies, but you’ll still pay income tax on withdrawals that aren’t used for medical expenses.)
8. Check your maximum HSA contribution.
You can contribute up to $3,850 to your HSA in 2023 if you have self-only coverage under an HDHP. If your HDHP also covers at least one other family member, you can contribute up to $7,750. And if you’ll be 55 or older by the end of the year, you can contribute an extra $1,000 to your HSA. You won’t pay income tax on the money you contribute, and you’ll also avoid FICA taxes if you make your HSA contributions as a payroll deduction.
If you had HDHP coverage in 2022 but haven’t hit the maximum HSA contribution yet, remember that you actually can make a contribution for 2022 any time prior to the April 15, 2023 tax filing deadline (the maximum contribution amounts for 2022 are $3,650 and $7,300, respectively).
9. If you don’t use it, don’t worry that you’ll lose it.
If you contribute money to your HSA and then don’t use it for medical expenses, it will roll over from one year to the next. Unlike flexible spending accounts, there’s no deadline for reimbursing yourself from your HSA. As long as your medical expense was incurred after you established the HSA – and you didn’t take the expense as an itemized deduction or receive reimbursement from another source – you can reimburse yourself years or decades later, after letting your HSA funds grow in the meantime.
Consider other financial tools
10. Assess your need for life insurance
If you have people counting on your income or other services that you provide, your untimely death could result in your loved ones having to deal with a reduced standard of living. If you don’t have life insurance, it’s worth reviewing your needs, especially if you’ve had any life changes recently, like getting married or having a child.
There are a variety of approaches to figuring out what level of life insurance coverage you need.
One easy way to estimate term life insurance needs is to simply multiply your income by anywhere from seven to ten times – and that method may be adequate for people who need fairly small amounts of life insurance coverage. That said, it can definitely be helpful to use a more in-depth calculator to pinpoint financial needs that you may have otherwise forgotten about.
If you use an online life insurance calculator, don’t be alarmed if the insurance carrier asks a long list of questions – some that might seem intrusive. Even if you’re looking for a quick, simple calculation, you’ll have to do a little homework to total your savings and investments.
(Life insurance is still medically underwritten; the ACA’s rules banning insurers from considering medical history do not apply to life insurance.)
Term life insurance isn’t the only option – there are other products available, including universal life insurance and whole life insurance. These are permanent life insurance policies, whereas a term policy has a set expiration date. If you buy a 30-year term life insurance policy and then you don’t die within the 30 years, your policy ends without ever paying any benefits (unless you purchased a return of premium rider). With a permanent policy, the plan can build cash value over time, and your beneficiaries will receive a payout regardless of when you die, as long as your policy remains in force.
Although permanent policies are useful in some situations, term life policies are much less expensive, and they’re adequate for most people’s needs.
11. Consider disability insurance
According to Social Security Administration data, a person who was born in 1998 has a 27% chance of being disabled at some point prior to age 67, whereas they only have a 6% chance of dying before age 67 (without ever being disabled).
If you were to become disabled, short-term or long-term, would you continue to be able to meet your financial obligations? Nearly six out of ten Americans don’t have enough in readily-available savings to cover a $500 emergency, and more than half of Americans live paycheck to paycheck.
If you and your family wouldn’t be able to get by without your income, you need to consider disability insurance as part of your overall financial plan. If you have a solid emergency fund, you might find that a long-term disability policy is enough. If not, you may want to consider both short-term and long-term disability coverage.
If you don’t have coverage through your employer, you can purchase private disability coverage, and there is a wide range of options available. More expensive policies tend to pay higher amounts and/or have shorter waiting periods (elimination periods) between when you become disabled and when the benefits begin. The level of coverage you’ll need will depend on factors like your monthly expenses, how much you have in savings, and whether your family has another source of income – there’s no one-size-fits-all.
Social Security also plays a role here; Social Security disability benefits currently provide income for more than 12 million Americans under the age of 65. But relying on Social Security alone might not be sufficient, depending on your situation. Social Security only provides disability benefits if your disability is long-term and you’re unable to do any work (not just unable to do the work you were doing before). You have to be disabled for at least five months before you can start receiving benefits, and the average benefit is less just a little over $1,200 per month.
The big picture
Health insurance, life insurance, and disability insurance are all part of a sound financial plan. If you’ve been ignoring some or all of them, now’s a good time to reevaluate your coverage options and get your financial house in order.
