Please provide your zip code to see plans in your area.
Featured

Featured

Medicaid expansion
What is Medicaid expansion?
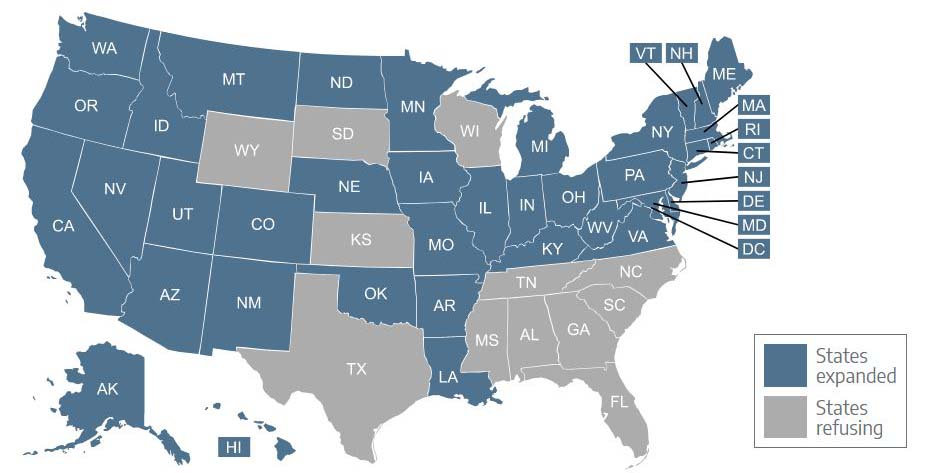
- Thirty-eight states and DC have expanded Medicaid under the ACA (South Dakota will join them in July 2023).
- Twelve states continue to refuse to adopt Medicaid expansion, despite the fact that the federal government will always pay 90% of the cost (this will drop to 11 once South Dakota’s Medicaid expansion takes effect).
- 21 million Americans had gained coverage as of 2022 through the ACA’s Medicaid expansion.
- The uninsured rate, particularly among low-income residents, is considerably lower in Medicaid expansion states.
What is Medicaid expansion?
A provision in the Affordable Care Act (ACA) called for the expansion of Medicaid eligibility in order to cover more low-income Americans. Under the expansion guidelines, Medicaid eligibility is extended to adults under the age of 65 with incomes up to 138% of the federal poverty level/FPL (133% plus a 5% income disregard).
Pre-ACA, Medicaid was generally never available to non-disabled adults under age 65 unless they had minor children. And even then, the income caps to qualify as a parent/caretaker were very low. By expanding Medicaid, the ACA created a viable pathway to coverage for millions of low-income adults.
Why are there some states that haven’t implemented Medicaid expansion?
The ACA called for Medicaid expansion nationwide. But in June 2012, the Supreme Court ruled that states could not be forced to expand their Medicaid programs, so it was left to each state to determine whether to participate or not.
When Medicaid expansion first took effect in 2014, it was only available in 26 states and DC. In the ensuing years, there has been a slow but steady increase in the number of states implementing Medicaid expansion. As of early 2023, Medicaid had been expanded in 38 states and the District of Columbia (see list below). Oklahoma and Missouri are the most recent states to have expanded Medicaid, both doing so in 2021. South Dakota will expand Medicaid in July 2023, under the terms of a ballot measure that voters approved in 2022 (South Dakota will be the seventh state to expand Medicaid due to a voter-approved ballot measure).
Wisconsin is not counted among the Medicaid expansion states, but the rules are different there. Wisconsin has implemented what essentially amounts to a partial expansion of Medicaid, and has no coverage gap (described below) because Medicaid is available to low-income adults with income below the poverty level.
But because Wisconsin has not fully expanded Medicaid as called for in the ACA (ie, Medicaid is not available in Wisconsin to adults with income between 100% and 138% of the poverty level), the state does not receive the enhanced federal Medicaid funding that it would receive if it fully expanded Medicaid.
Georgia plans to partially expand Medicaid in the summer of 2023, using an approach similar to Wisconsin’s (ie, it would still count as a non-expansion state), and also incorporating a work requirement. Like Wisconsin, Georgia will forego the enhanced federal funding that would be available if the state were to fully expand Medicaid.
How is Medicaid expansion funded?
The federal government is financing most of the cost of expanding Medicaid, and a small portion is being paid by participating states. The costs for enrollees who are newly eligible under the expanded guidelines were covered 100% by the federal government until the end of 2016. The states then gradually started paying a portion of the cost, reaching 10% by 2020.
The funding will remain at the 90/10 split going forward, with the federal government always paying 90% of the cost of covering the population that became newly eligible due to the expansion of Medicaid.
The states that refuse to expand Medicaid only receive their normal federal Medicaid funding, rather than the enhanced 90% funding that they would receive to cover the newly eligible population if they were to expand coverage (in the Medicaid expansion states, the normal federal funding still applies for the populations that were already eligible pre-expansion).
As noted above, the federal government does not provide this funding unless a state fully expands Medicaid. So Wisconsin continues to receive its normal federal match for Medicaid funding, and Utah was unable to secure Medicaid expansion funding until Medicaid was fully expanded (Utah initially implemented a partial expansion of Medicaid, but did not receive enhanced federal funding for it). Georgia plans to implement a partial Medicaid expansion, and will not be eligible for enhanced federal funding to pay for it.
How many people are enrolled in coverage due to Medicaid expansion?
As of 2019, there were about 10 million people who had become newly eligible for Medicaid due to the ACA’s expanded eligibility guidelines. But the COVID pandemic drove the enrollment numbers significantly higher: As of 2022, there were about 21 million Medicaid enrollees who had gained eligibility due to Medicaid expansion.
Total enrollment in Medicaid/CHIP has increased by 59% since 2013 (a growth of more than 34 million people), and that includes the dozen states that have continued to reject federal funding to expand Medicaid.
Medicaid expansion has played a large role in the increase, but the growth has also been driven by the fact that Medicaid disenrollments have been paused since the start of the COVID pandemic. This means enrollment has continued to increase without any of the disenrollments that would normally occur when people lose eligibility for Medicaid due to a change in circumstances. This will end starting in April 2023, when states resume routine Medicaid eligibility redeterminations and begin disenrolling people who are no longer eligible .
What is the Medicaid coverage gap?
In the states that have not expanded Medicaid, there’s a coverage gap that leaves about 2 million people ineligible for any sort of affordable coverage. These people are not eligible for premium subsidies in the marketplace because their income is under the poverty level. But they are also ineligible for Medicaid because their states have refused to implement Medicaid expansion.
According to US Census data, the percentage of people below the poverty level who are uninsured is more than twice as high in states that haven’t expanded Medicaid, compared with states that have. To be clear, this is due to the decisions that their states have made, rather than a flaw in the ACA itself. The states could opt to accept federal funding to expand Medicaid at any time, thus closing the coverage gap.
Five states — Texas, North Carolina, Florida, Georgia, and Tennessee — account for the lion’s share of the coverage gap population, and they are among the 12 states where Medicaid expansion is still a contentious issue and the legislature and/or governor are still strongly opposed to accepting federal funding to expand Medicaid.
(Note that South Dakota will expand Medicaid in mid-2023, and North Carolina lawmakers might reach an agreement in 2023 that would allow the state to expand Medicaid. As noted above, Georgia plans to partially expand Medicaid in mid-2023, but with a work requirement. So the number of people expected to become eligible for Medicaid in Georgia is just a fraction of what it would be with full Medicaid expansion without a work requirement.)
For people in the coverage gap who received unemployment compensation for at least one week in 2021, the American Rescue Plan provided eligibility for premium subsidies. But this was a temporary provision for 2021.
The Build Back Better Act would have provided federal subsidies for four years to people in the coverage gap, allowing them to purchase premium-free coverage with enhanced benefits that leave them with very little out-of-pocket costs. That legislation passed the House in the fall of 2021, but stalled in the Senate due to objections from all GOP Senators as well as two Democrats.
There were ongoing negotiations in 2022 about federal funding to close the Medicaid coverage gap. But ultimately, the Inflation Reduction Act was enacted in 2022 without any provision to close the Medicaid coverage gap (it did, however, extend some of the American Rescue Plan subsidy enhancements, and also provided significant benefit improvements for people with Medicare drug coverage).
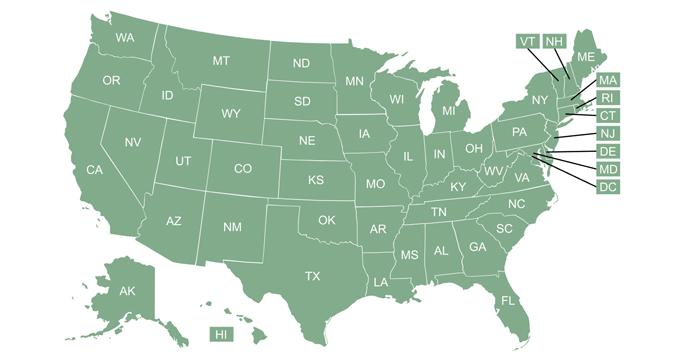
Which states have expanded Medicaid?
As of early 2023, Medicaid has been expanded in 38 states and Washington, D.C. (you can click on a state on this map for more information about each state):
- Alaska
- Arizona
- Arkansas
- California
- Colorado
- Connecticut (for parents, eligibility extends to 160% FPL)
- Delaware
- Hawaii
- Idaho
- Illinois
- Indiana
- Iowa
- Kentucky
- Louisiana
- Maine
- Maryland
- Massachusetts
- Michigan
- Minnesota
- Missouri
- Montana
- Nebraska
- Nevada
- New Hampshire
- New Jersey
- New Mexico
- New York
- North Dakota
- Ohio
- Oklahoma
- Oregon
- Pennsylvania
- Rhode Island
- South Dakota will join this list as of July 2023
- Utah
- Vermont
- Virginia
- Washington
- Washington, D.C. (eligibility extends to 215% FPL)
- West Virginia
Which states have refused to expand Medicaid?
As of early 2023, the following states have not yet accepted federal funding to expand Medicaid:
- Alabama
- Florida
- Georgia (partial expansion in mid-2023, with a work requirement)
- Kansas
- Mississippi
- North Carolina
- South Carolina (no coverage gap for parents of minor children)
- South Dakota (Medicaid expansion takes effect July 2023)
- Tennessee (very little coverage gap for parents of minor children)
- Texas
- Wisconsin (no coverage gap)
- Wyoming
Related articles
Get updated information on the current status of Medicaid expansion, along with general information about each state’s program.